Saint Francis College, Brooklyn Heights, New York. U. Leif, MD: "Buy Aciclovir online - Trusted online Aciclovir no RX".
Randomized controlled trials comparing midsuburethral tapes and pubovaginal slings had similar efficacy in terms of both overall and subjective continence rate [10] cheap 400 mg aciclovir visa hiv infection rates in thailand. With regard to complication order aciclovir 800mg on-line pharmacology antiviral quiz, the risk of intraoperative bladder perforation were significantly lower in the pubovaginal sling group; pelvic hematoma was similar in the two procedures generic aciclovir 200 mg visa antiviral tablets. However discount aciclovir 400mg overnight delivery antiviral research, midsuburethral tapes were followed by a significantly lower risk of storage symptoms and reoperation. Intraoperative Complications In case of bladder injury, localizing precisely the injuries by opening the bladder dome allows to repair and does not prevent from implanting the device if correctly repaired [40,42]. It is of trained center expert opinion that any injury at the level of the bladder neck or posterior urethral portion indicates not to implant the device. Any bladder injury far away from the bladder neck, either involuntary or voluntary done as an eye control of dissection, do not contraindicate implantation of the cuff. Vaginal injury is rare and leads to stop the procedure when it is located posteriorly to the bladder neck and/or urethra, in front of cuff placement. Any vaginal injury (lateral on cul-de-sac) may not stop the surgery and must be carefully repaired. Postoperative Period Postoperative acute urinary retention can occur and leads to a new indwelling catheter insertion for at least 48 hours [40]. Usually, it is of interest to let a catheter until day 5 or 6 to decrease recatheterization rate. The main long-term complications of an artificial urinary sphincter is explantation of the device in 3%–50% of cases due to infection and/or erosion [43–45] and the need for revision of the device in 13%–63% of cases [43]. The major reported risk factors for explantation are aging, previous anti-incontinence procedures, a delay between the previous procedure and sphincter implantation, perioperative complications, and pelvic irradiation [43,46–48]. The revision rates after 5 years reported in the literature range from 13% to 63%. Most of revisions were due to the mechanical failure of the pump, balloon, cuff, or connections (Figure 80. Discrepancies between series may also be related to the medical histories of irradiation among the women [44], the number of previous anti- incontinence procedures before the insertion of the artificial urinary sphincter [39], or learning curves and the surgeon’s experience. The artificial urinary sphincter is supposed to have an average life span of 10 years. According to the American and European Guidelines, the exact indication and the optimum timing for artificial urinary sphincter implantation in women are not clear [52,53]. A group of experts attempted to clarify and optimize 1230 indication and technique [41]. But the place of this therapy in the decision tree for female urinary incontinence management has not been clearly defined at this moment in international guidelines [52]. Most intraoperative complications are urethral or bladder perforations, observed in 3%– 17% of cases. Postoperative complications, during the first year, includes urethral erosion (2%–15%), cutaneous erosion of the port (3%–7. Other reported complications are less frequent: labial hematoma, labial infection, urinary infection, de novo urgency, dyspareunia, dysuria, pain, and discomfort. Periurethral injections can sometimes have lasting effects, but repeated injections may be necessary [64,65]. Potential local side effects include urinary tract infection, urinary retention, local pain, pseudo-abscess formation, and urethral erosion. Distant effects as a result of particle migration are generally site specific and include pulmonary embolism. The incidence of urinary retention following the procedure ranges from 15% to 25% [66–68]. In case of persistent obstruction, resection of the implanted material may be performed [70] (Figure 80. In conclusion, this technique can be used because of its good benefit/risk balance in frail patients, previously operated patients, and patients refusing surgery. The International Urogynecological Association and the International Continence Society recognized the increasing use of prostheses (meshes) and grafts in female pelvic floor surgery [71]. The classification was developed to be sensitive to all possible physical complications involving the use of a prosthesis or graft in a female pelvic floor surgical procedure. Complications were classified according to three aspects: category, time, and site. Indeed, complications involving the use of meshes, tapes, and grafts in female pelvic floor surgery need to involve the following viewpoints of (1) local complications, (2) complications to surrounding organs, and (3) systemic complications. A key advantage of a standardized classification is that all parties involved in female pelvic floor surgery including surgeons, physicians, nurses, allied health professionals, and industry will be referring to the same clinical issue. Careful counseling allowing realistic patient expectations with regard to complications will set a benchmark from the perspective of the most important outcome, namely, patient satisfaction. The standardisation of terminology of lower urinary tract function: Report from the standardisation sub-committee of the International Continence Society. Complications of mid urethral slings: Important outcomes for future clinical trials. Retropubic compared with transobturator tape placement in treatment of urinary incontinence: A randomized controlled trial. Complications of tension-free vaginal tape surgery: A multi- institutional review. Updated systematic review and meta-analysis of the comparative data on colposuspensions, pubovaginal slings, and midurethral tapes in the surgical treatment of female stress urinary incontinence. Lower urinary tract injuries after transobturator tape insertion by different routes: A large retrospective study. Peri-operative complications and pain after the suburethral sling procedure for urinary stress incontinence: A French prospective randomised multicentre study comparing the retropubic and transobturator routes. Tension-free vaginal tape procedure for the treatment of female stress urinary incontinence: Long-term results. Complications and short-term results of two different transobturator techniques for surgical treatment of women with urinary incontinence: A randomized study. Surgical complications and medium-term outcome results of tension-free vaginal tape: A prospective study of 313 consecutive patients. Surgical treatment of female stress urinary incontinence with a trans-obturator-tape (T. Transobturator and retropubic tape procedures in stress urinary incontinence: A systematic review and meta-analysis of effectiveness and complications. Erosions and urinary retention following polypropylene synthetic sling: Australasian survey. A comparison of bladder neck movement and elevation after tension-free vaginal tape and colposuspension. Comparison of tension-free vaginal taping versus modified Burch colposuspension on urethral obstruction: A randomized controlled trial. Laparoscopic surgical complete sling resection for tension-free vaginal tape-related complications refractory to first-line conservative management: A single-centre experience. Anatomical study of the obturator foramen and dorsal nerve of the clitoris and their relationship to minimally invasive slings.
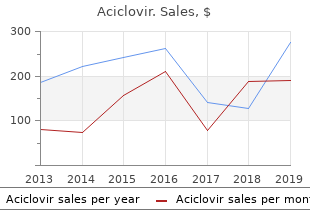
Stroke index values were statistically analyzed for two samples of patients suffering from myocardial infarction order 400mg aciclovir mastercard antiviral lubricant herpes. Construct the 95 percent confidence interval for the ratio of the two population variances buy aciclovir 200 mg fast delivery hiv infection rate in sierra leone. Thirty-two adult asphasics seeking speech therapy were divided equally into two groups cheap 400 mg aciclovir with mastercard hiv infection from undetectable. Statistical analysis of the treatment effectiveness scores yielded the following variances: s2 ¼ 8; s2 ¼ 15 buy cheap aciclovir 200 mg on-line antiviral natural factors. Sample variances were computed for the tidal volumes (milliliters) of two groups of patients suffering from atrial septal defect. The results and sample sizes were as follows: n ¼ 31; s2 ¼ 35; 000 1 1 n ¼ 41; s2 ¼ 20; 000 2 2 Construct the 95 percent confidence interval for the ratio of the two population variances. Glucose responses to oral glucose were recorded for 11 patients with Huntington’s disease (group 1) and 13 control subjects (group 2). Statistical analysis of the results yielded the following sample variances: s2 ¼ 105; s2 ¼ 148. Construct the 95 percent confidence interval for the ratio of the two 1 2 population variances. Measurements of gastric secretion of hydrochloric acid (milliequivalents per hour) in 16 normal subjects and 10 subjects with duodenal ulcer yielded the following results: Normal subjects: 6. The concepts and methods involved in the construction of confidence intervals are illustrated for the following parameters: means, the difference between two means, proportions, the difference between two proportions, variances, and the ratio of two variances. In addition, we learned in this chapter how to determine the sample size needed to estimate a population mean and a population proportion at specified levels of precision. We learned, also, in this chapter that interval estimates of population parameters are more desirable than point estimates because statements of confidence can be attached to interval estimates. Define the following: (a) Reliability coefficient (b) Confidence coefficient (c) Precision (d) Standard error (e) Estimator (f) Margin of error 6. What are the assumptions underlying the use of the t distribution in estimating a single population mean? What are the assumptions underlying the use of the t distribution in estimating the difference between two population means? Arterial blood gas analyses performed on a sample of 15 physically active adult males yielded the following resting PaO2 values: 75; 80; 80; 74; 84; 78; 89; 72; 83; 76; 75; 87; 78; 79; 88 Compute the 95 percent confidence interval for the mean of the population. Of 70 manufacturing plants of a certain type visited, 21 received a “poor” rating with respect to absence of safety hazards. Construct a 95 percent confidence interval for the population proportion deserving a “poor” rating. How large a sample would be required to estimate the population proportion to within. In a dental survey conducted by a county dental health team, 500 adults were asked to give the reason for their last visit to a dentist. Of the 220 who had less than a high-school education, 44 said they went for preventative reasons. Of the remaining 280, who had a high-school education or better, 150 stated that they went for preventative reasons. Construct a 95 percent confidence interval for the difference between the two population proportions. A breast cancer research team collected the following data on tumor size: Type of Tumor n x s A 21 3. A certain drug was found to be effective in the treatment of pulmonary disease in 180 of 200 cases treated. Seventy patients with stasis ulcers of the leg were randomly divided into two equal groups. At the end of the experiment, treatment effectiveness was measured in terms of reduction in leg volume as determined by water displacement. The means and standard deviations for the two groups were as follows: Group (Treatment) x s A cc B 125 cc 30 Construct a 95 percent confidence interval for the difference in population means. What is the average serum bilirubin level of patients admitted to a hospital for treatment of hepatitis? A sample of 10 patients yielded the following results: 20:5; 14:8; 21:3; 12:7; 15:2; 26:6; 23:4; 22:9; 15:7; 19:2 Construct a 95 percent confidence interval for the population mean. Determinations of saliva pH levels were made in two independent random samples of seventh-grade schoolchildren. Sample A children were caries-free while sample B children had a high incidence of caries. An independent random sample of 16 patients with the same complaint received drug B. The number of hours of sleep experienced during the second night after treatment began were as follows: A: 3. For the 52 women who received oral misoprostol, the mean time in minutes to active labor was 358 minutes with a standard deviation of 308 minutes. For the 53 women taking oxytocin, the mean time was 483 minutes with a standard deviation of 144 minutes. Construct a 99 percent confidence interval for the difference in mean time to active labor for these two different medications. Over a 2-year period, 34 European women with previous gestational diabetes were retrospectively recruited from West London antenatal databases for a study conducted by Kousta et al. Women older than 65 years of age who were long-term residents were invited to participate if they had no diagnosis of terminal cancer or metastatic disease. Construct a 95 percent confidence interval for the percent of women with vitamin D deficiency in the population presumed to be represented by this sample. In a study of the role of dietary fats in the etiology of ischemic heart disease the subjects were 60 males between 40 and 60 years of age who had recently had a myocardial infarction and 50 apparently healthy males from the same age group and social class. The data on this variable were as follows: Subjects with Myocardial Infarction Subject L. What do these data suggest about the levels of linoleic acid in the two sampled populations? The purpose of a study by Tahmassebi and Curzon (A-33) was to compare the mean salivary flow rate among subjects with cerebral palsy and among subjects in a control group. The following table gives the mean flow rate in ml/minute as well as the standard error. Curzon, “The Cause of Drooling in Children with Cerebral Palsy—Hypersalivation or Swallowing Defect? Construct the 90 percent confidence interval for the difference in mean salivary flow rate for the two populations of subjects represented by the sample data. Thirty-six women took part in the study with 19 in the Burch treatment group and 17 in the sling procedure treatment group. One of the outcome measures at three months post-surgery was maximum urethral closure pressure (cm H2O).
Why and how are etiological and pathophysiological issues which are illustrated in this chapter discount 200mg aciclovir fast delivery hiv infection history. Surgical treatment of an enterocele is often concurrent or identical to operations for vaginal vault prolapse buy 200 mg aciclovir mastercard pictures of hiv infection symptoms. Therefore buy aciclovir 200mg fast delivery hiv infection no symptoms, the pouch of Douglas is an anatomical structure that plays an important and probably predisposing part order 200mg aciclovir otc hiv infection without penetration. The pouch of Douglas is normally closed and does not contain intestine or omentum. In anatomy textbooks, the extent of the pouch of Douglas has traditionally been described as 2–3 cm below the uterosacral ligaments (e. Histological studies by Uhlenhuth and colleagues have demonstrated that in the fetus the pouch of Douglas may extend to the perineal body [3]. The consecutive fusion of the anterior and posterior peritoneum forms the rectovaginal septum and determines the depth of the pouch of Douglas [3–5]. According to Uhlenhuth, the rectovaginal septum is distinguishable from the “fascial” capsule of the vagina and rectum. In contrast to anatomy textbooks, intra-abdominal measurements of the depth of the pouch of Douglas in young nulliparous women revealed great variations with 25%–75% of the posterior vaginal wall covered with peritoneum [6]. The mean depth of the pouch of Douglas was 49% of vaginal length in nulliparas, 46% in parous women, and was significantly deeper (72%) in patients with posterior vaginal wall prolapse. It would appear that the deep pouch of Douglas is frequently present in young nulliparous women without pelvic organ prolapse, which implies a congenital variation and predisposition [6]. A sophisticated concept of normal pelvic organ support accentuates the imperative role of several factors including integrity of the anterior and posterior endopelvic fascia with intact attachments as well as normal tone, position, and functionality of the levator ani muscle. Normal pelvic floor muscle and fascial structures are required to hold the perineum in place and ensure normal bladder, bowel, and sexual function. It is apparent that fascial defects in the three levels of vaginal support and the posterior compartment may contribute to pelvic organ prolapse including enteroceles [7,8]: the normal pelvic floor tone is essential for the nearly horizontal axis of the vagina, which in turn is necessary to allow for a normal pelvic floor protecting intra-abdominal pressure distribution. Intra-abdominal measurements of the depth of the pouch of Douglas have shown that in women with posterior vaginal 1268 wall and anterior rectal wall prolapse the pouch of Douglas is significantly deeper and may reach the level of the perineal body [6]. In addition, the anatomy of the pouch of Douglas is considerably different, which is a recognized feature in some studies. In women with severe pelvic organ prolapse, a large or voluminous rectovaginal pouch was a consistent anatomic finding, requiring obliteration during pelvic reconstructive surgery [9–11]. Apart from a mobile vaginal axis and a dehiscence of the levator hiatus, French authors reported a “grande fosse pelvi-périnéale”—a large pelvic pouch—to be the principal lesion in women with enteroceles [12]. Other authors described this phenomenon as an abnormally deep and wide cul-de-sac with a 3D enlargement [13]. Their anatomical observations included a deep and wide rectovaginal pouch and a rectosigmoid colon, which closely follows the sacral curve (Figure 83. Although different positions and courses of the sigmoid colon and its mesentery are known [14], systematic descriptions in women with pelvic organ prolapse are scarce. Baessler and Schuessler found 64% of women with enteroceles and all women with anterior rectal wall procidentia to have these features, termed as “grande fosse pelvienne. Given these findings, it seems reasonable to regard a deep pouch of Douglas as a risk factor for enterocele formation. An enterocele can only develop when other factors open and expose the deep pouch of Douglas. Normal pelvic floor support prevents opening and exposure of the pouch of Douglas. Vaginal Axis In a woman with normal pelvic organ support, the pouch of Douglas is closed, irrespective of its depth, and lies nearly horizontally between the levator plate and the vagina [16–18]. It is known that operations that change the vaginal axis can lead to increased prolapse in the “unprotected” area. This is true for the higher incidence of cystoceles after sacrospinous fixations, where the position of the vagina is more posterior and also for the considerate rate of rectoceles and enteroceles after Burch colposuspensions or ventrofixations where the vagina is displaced anteriorly. A further process that changes the vaginal axis is excessive perineal descent (or descending perineum syndrome), which is often seen clinically in women with significant posterior vaginal wall prolapse (Figure 83. A deep pouch of Douglas is likely to accentuate the process of enterocele development once the vaginal axis is changed. Endopelvic “Fascia” The integrity of the anterior and posterior endopelvic fascia or connective tissue and its attachments is essential for normal pelvic organ support [8]. A defect in the endopelvic fascia or insufficiency is necessary for an enterocele to protrude. However, an intact endopelvic connective tissue might only prevent the enterocele from bulging into the vagina but not into the rectum causing an anterior rectal wall procidentia (Figure 83. It is not entirely apparent whether the endopelvic fascia is identical to the rectovaginal septum as the latter can be rather short [20], depending on the depth of the pouch of Douglas. Whole-thickness biopsies of the leading edge of radiologically proven enteroceles showed that in none of the 13 women examined the vaginal epithelium was in direct contact with the perineum and all had a well-defined vaginal wall muscularis [21]. These findings add to the ongoing controversy on whether the fascia exists or not. It has been suggested that it is a structure that is artificially created during surgical dissection. This debate is complicated by inconsistent histological studies, some of which do not substantiate the concept of a fascia between the rectum and vagina. However, it might simply be a question of definition: the fascia is a connective tissue usually with smooth muscle cells and it might also contain fatty or areolar tissue [22] (Figure 83. Whether the fascia is part of the vagina or rectum or whether it is a separate structure is of scientific but not clinical value. Fascia in the clinical sense means connective tissue that has tensile strength and is strong enough to hold sutures and support the underlying organs. These photos demonstrate a nearly normal position of the perineum at rest (a) but a “ballooning” of the perineum on straining (b). This patient had a large rectoenterocele that did not protrude outside the introitus. This stain is used to differentiate fibrous tissue (green) and smooth muscle (red). Note the amount of smooth muscle, organized connective tissue, and areolar tissue. Apart from bowel symptoms, which can be similar to complaints of patients with rectoceles or enteroceles, excessive perineal descent of more than 2 cm (measured in relation to the ischial tuberosities) is seen more frequently in women with posterior vaginal wall prolapse [24]. Solitary rectal ulcer, rectal prolapse, and intussusception are common concomitant findings [24,25]. The etiology is unclear, but reduced pelvic floor tone [26] with insufficient perineal and endopelvic fascial attachment and a deep pouch of Douglas and sigmoid colon elongation have been discussed. The term “ballooning” is also used to describe an enlargement of the genital hiatus during straining on perineal 3D ultrasound and is associated with pelvic organ prolapse [27]. Pulsion, Traction, Sliding, True, and Congenital: Concepts of Enterocele Development There are different concepts, and each one of them might be true in an individual patient.
Either form of heparin should be started 2 hours before surgery and the compression stockings placed on the patient in the operating room before incision buy 800 mg aciclovir amex antiviral lip balm. The abdomen 400mg aciclovir otc hiv infection us, vagina 200mg aciclovir with amex antiviral y antibiotico juntos, and perineum are sterilely prepped and draped order aciclovir 800mg with visa hiv infection greece, and a 16 Fr Foley catheter with a 10 mL balloon is inserted for easy identification of the bladder neck. If a vaginal hysterectomy has been performed, the incised apex of the anterior vaginal wall is grasped transversely with two Allis clamps and elevated. Otherwise, a transverse or diamond-shaped incision is made in the vaginal epithelium near the apex. A third Allis clamp is placed about 2 cm below the posterior margin of the urethral meatus and pulled up. If a midurethral sling is to be done, then the incision is only made to the bladder neck; a separate incision is made for the sling. Additional Allis clamps may be placed in the midline between the urethra and apex. Alternatively, the points of a pair of curved Mayo scissors are inserted between the vaginal epithelium and the vaginal muscularis, or between the layers of the vaginal muscularis, and gently forced upward while being kept half opened/half closed (Figure 82. Countertraction during this maneuver is important to minimize the likelihood of perforation of the bladder. The vagina is incised in the midline, and the incision is continued to the level of the midurethra (or bladder neck if a sling is being done). As the vagina is incised, the edges are grasped with Allis or T-clamps and drawn laterally for further mobilization. Dissection of the vaginal flaps is then accomplished by turning the clamps back across the forefinger and incising the vaginal muscularis with a scalpel or Metzenbaum scissors, as shown in Figure 82. An assistant maintains 1253 constant traction medially on the remaining vaginal muscularis and underlying vesicovaginal adventitia. This procedure is performed bilaterally until the entire extent of the anterior vaginal prolapse has been dissected; in general, the dissection should be carried further laterally with more advanced prolapse. The spaces lateral to the urethrovesical junction are sharply dissected toward the ischiopubic rami. It is also important to use sharp dissection to mobilize the bladder base from the vaginal apex as shown in Figure 82. If the patient does not suffer from stress urinary incontinence, plicating sutures at the urethrovesical junction could be placed to augment posterior urethral support and to help ensure that stress incontinence, if not present at the time of operation, does not develop postoperatively. Although it may help to prevent de novo stress incontinence, it can also lead to voiding difficulty after surgery. Vesical neck plication was used to treat mild stress urinary incontinence in the past but is no longer done for that indication. Once the vaginal flaps have been completely developed, the urethrovesical junction can be identified visually or by pulling the Foley catheter downward until the bulb obstructs the vesical neck. The first plicating stitch is placed into the periurethral endopelvic fascia and tied (Figure 82. One or two additional stitches are placed to support the length of the urethra and urethrovesical junction. Depending on the severity of the prolapse, one or two rows of plication sutures or a purse-string suture followed by plication sutures are placed (Figure 82. The vaginal epithelium is then trimmed from the flaps bilaterally, and the remaining anterior vaginal wall is closed with a running No. Anti-incontinence operations are often performed at the same time as anterior vaginal prolapse repair to treat coexistent stress incontinence, although this practice is somewhat controversial and varies in different geographic regions. Suburethral bladder neck sling placement may also improve the cure rate of the prolapse [26]. Bladder neck suspension procedures (pubovaginal sling procedures or retropubic colposuspension) effectively treat mild anterior vaginal prolapse associated with urethral hypermobility and stress incontinence. More advanced anterior vaginal prolapse will not be treated adequately and, in these cases, anterior colporrhaphy or anterior vaginal mesh repair should be performed, often in conjunction with a colpopexy procedure and a midurethral sling. Surgical judgment is required to perform the bladder plication tightly enough to reduce the anterior vaginal prolapse sufficiently, yet preserve some mobility of the anterior vagina. If anterior colporrhaphy is combined with a sling procedure (midurethral or bladder neck), the cystocele should be repaired before the final tension is set for the sling. Randomized trials support concurrent placement of a midurethral sling at the time anterior vaginal prolapse surgery even in continent women in order to prevent de novo stress urinary incontinence after surgery [22]. A midurethral sling, such as a tension-free vaginal tape or transobturator sling, is best done through a separate midurethral incision after the cystocele repair is complete. This can be done in a number of ways and the surgical techniques continue to evolve. Biological materials that have been used include autografts of harvested rectus fascia and fascia lata, human allografts including fascia lata and dura mater, and xenografts such as porcine dermis, porcine small intestinal submucosa, and bovine pericardium. In 2010, approximately 25% of surgeries for pelvic organ prolapse in the United States included transvaginal placement of biologic or synthetic mesh. Many surgeons use transvaginal graft placement in an attempt to increase the efficacy and durability of their surgical repair. For anterior prolapse, studies have demonstrated improved anatomic outcomes after transvaginal placement of permanent synthetic mesh when compared to anterior colporrhaphy without mesh (“native-tissue repair”) [27]. However, this comes at the expense of an increased rate of complications unique to synthetic mesh placement including longer operating time and higher blood loss, vaginal mesh exposure or extrusion, mesh erosion or perforation into an adjacent organ (bladder, urethra, or rectum), and vaginal mesh contraction with associated pain and dyspareunia [27]. Sharp dissection is used to mobilize the bladder base from the vaginal apex during anterior colporrhaphy. When considering the use of transvaginal mesh for anterior prolapse, surgeons and patients must balance improved anatomic support of the anterior vaginal wall against the cost of the devices and increased complications such as mesh erosion, exposure, or extrusion, pelvic pain, groin pain, and dyspareunia. In a joint Committee Opinion published in December 2011, the American Urogynecologic Society and the American College of Obstetrics and Gynecology recommended that pelvic organ prolapse vaginal mesh repair should be reserved for high-risk individuals in whom the benefit of mesh placement may justify the risk, such as individuals with recurrent anterior prolapse or with medical comorbidities that preclude more invasive and lengthier open and endoscopic procedures [28]. They also noted that surgeons placing vaginal mesh should undergo training specific to each device and have experience with reconstructive surgical procedures and a thorough understanding of pelvic anatomy. Prior to considering treating the anterior vaginal prolapse with graft or mesh, patients should undergo a thorough informed consent process including discussion of risks, benefits, and both surgical and nonsurgical alternative treatments. Many surgeons would not consider the use of mesh in a patient who has had a previous mesh complication. Mesh augmentations should not be used in pregnant women or women who are contemplating future pregnancy, as the vaginal mesh does not stretch significantly. In patients who have had pelvic radiation, mesh placement is not recommended because of the risk of poor wound healing. Similarly, preexisting local or systemic infection is a contraindication for vaginal mesh placement, particularly nonabsorbable synthetic mesh. Many surgeons would not recommend the use of nonabsorbable synthetic mesh if colorectal surgery is being performed concurrently. Chronic steroid use, smoking, uncontrolled diabetes mellitus, or other causes of a compromised immune system can impair wound healing, and many would consider these conditions to be relative contraindications to vaginal mesh placement. Pelvic pain syndromes such as endometriosis, vulvodynia, interstitial cystitis, fibromyalgia, and dyspareunia should be evaluated preoperatively to allow for comprehensive counseling as to the best surgical and nonsurgical form of treatment.
The skin of the scalp is the thickest skin of the body order aciclovir 800mg on-line hiv infection blood splash, rang- This space is considered the “danger zone” of the scalp ing from 8 mm in the occipital region to 3 mm in the anterior because hematoma or infection can easily spread through it trusted 800 mg aciclovir graphs on hiv infection rates, and temporal regions aciclovir 400 mg lowest price hiv infection and seizures. It consists of The innermost layer of the scalp aciclovir 800 mg for sale hiv infection more condition symptoms, the pericranium, is adipose tissue and fibrous connective tissue organized in firmly connected to the outer table of the skull. It has a quadrilat- consists of a superficial layer that adheres to the lateral eral shape, and therefore has a superficial and a deep face border of the zygomatic arch, and a deep layer that adheres and four margins, anterior, posterior and two laterals. The superfi- The superficial face is firmly connected to the overlying cial temporal adipose tissue is located between the two structures through the septa that pass across the subcutane- layers. The deep face is separated from the pericranium by a deep layer of avascular connective tissue. The scalp is highly vascularized by four main arteries and It originates from the anterior margin of the galea and runs smaller vessels. The main arteries are the occipital and super- anteriorly and downward until the deep face of the skin in ficial temporal arteries on each side. The smaller vessels of correspondence with the eyebrows, glabella, and superior the scalp are the posterior auricular artery, small branches of portion of the dorsum of nose, where it inserts. It interdigi- the posterior auricular artery, small branches of the external tates with fibers from the procerus, corrugator supercilii, and carotid artery, and supraorbital and supratrochlear vessels. The frontalis muscle, by contract- These vessels are contained in the subcutaneous layer and ing, moves the scalp forward and causes frowning. Its fibers run obliquely, medially, and downward to insert on the posterior nuchal line and the mastoid process. The occipital artery arises from the external carotid artery The anterosuperior auricular muscle is located in the tem- above the origin of the lingual artery and runs posteriorly, poral region, forward and superiorly to the auricula. It origi- upward, and outward, passing beneath the posterior belly of nates from the lateral margin of the galea and inserts on the the digastric muscle and then in the groove of the mastoid lateral face of the auricula in correspondence with the helix, process. It pierces the fascia connecting the cranial attach- the spine of the helix, and the anterosuperior part of the con- ment of the trapezius and sternocleidomastoid muscles, and vexity of the concha. Along its course it posterior, between which runs the parietal branch of the ante- divides into the following branches: rior superficial temporal artery. The frontalis, occipitalis, and anterosuperior auricular • Muscular branches for the sternocleidomastoid, digastric, muscles are intrinsic muscles and belong to the group of stylohyoid, splenius, and longissimus capitis muscles mimic muscles. The superficial portion anastomoses Its terminal branches are: with the transverse cervical artery. The deep portion anastomoses with the vertebral and deep cervical arteries • Frontal (anterior) branch, which supplies the frontal region • Meningeal branches, which enter the skull through the • Parietal (posterior) branch, which supplies the skin and jugular foramen and condyloid canal, to supply the dura the epicranial aponeurosis of the parietal region mater in the posterior fossa The terminal branches of the occipital artery are the 6. These branches, with a tortuous course, anastomose to the contra- The supratrochlear and supraorbital arteries supply the ante- lateral occipital branches and the branches of the superficial rior region of the scalp. The supraorbital artery passes between the superior rectus muscle and levator palpebrae superioris muscle, to the apex of the orbit. The posterior auricular artery arises above the posterior belly The supratrochlear artery is one of the terminal branches of the digastric muscle, and ascends in the groove between of the ophthalmic artery. It enters the facial canal through the The supratrochlear and supraorbital arteries anastomose stylomastoid foramen and supplies the mastoid cells, the sta- in the frontoparietal subcutaneous layer of the scalp. The extracranial venous circulation is connected to the intracranial venous circulation through several emissary The superficial temporal artery is the most important vessel veins. The emissary veins, after passing through the cranial of the scalp because of its length and surface supply. The venous system of the in the substance of the parotid gland, behind the neck of the scalp follows the arterial one. In the temporal The frontal, supraorbital, and nasofrontal veins unite region, beneath the skin, it divides into a frontal and a pari- superficially at the medial angle region of the eye to form the etal branch. When it passes anterior to the tragus it is only angular vein, which runs obliquely downward and backward covered by the skin, and its pulse is palpable (pulsatility). It with a linear course, receiving numerous branches to become is accompanied by the corresponding vein and the auriculo- the anterior facial vein. Its collateral branches are: The union of the superficial temporal vein and the middle temporal vein, anterior to the auricle, forms the posterior • Parotid branches for the parotid gland facial vein. Its area corresponds to that of the superficial tem- • Transverse facial artery poral artery. The frontal nerve, the largest terminal branch of the ophthalmic nerve, enters the The scalp has numerous sensitive nerves. The supraorbital orbital cavity through the superior orbital fissure, external to and supratrochlear nerves, terminal branches of the ophthal- the tendinous ring (annulus of Zinn). It runs along the apex mic division of the fifth cranial nerve, innervate the anterior of the orbital cavity in close contact with the periosteum, From the ophthalmic division of trigeminal nerve (V1) Supraorbital nerve Supratrochlear nerve Auricular branch of vagus nerve (X) Palpebral branch of lacrimal nerve Infratrochlear nerve External nasal branch of anterior ethmoidal nerve From the maxillary Medial branches division of trigeminal of posterior divisions nerve (V2) of cervical spinal nerves Zygomaticofacial nerve Greater occipital nerve (C2) Zygomaticotemporal Third occipital nerve (C3) nerve Spinal nerves C4, C5, C6, C7 Infraorbital nerve and C8 From the mandibular Branches of cervical plexus division of trigeminal Lesser occipital nerve (V3) nerve (C2,C3) Mental nerve Great auricular Buccal nerve nerve (C2, C3) Transverse cervical (or Auriculo-temporal nerve cutaneous cervical) nerve (C2, C3) Posterior divisions of cervical spinal nerves Ophtalmic nerve (V1) Auricular branch of vagus nerve to the external acoustic Trigeminal meatus and small area of nerve (V) Maxillary nerve (V2) postero-medial aspect of the auricula Mandibular nerve (V3) Branches of cervical plexus Fig. Along its course dible, and reaches the parotid lodge, passing through the on the orbital margin it divides into the supratrochlear, fron- parotid gland. It turns superiorly, outward, between the external auditory The supratrochlear branch is the smallest and most medial meatus and the superficial temporal vessels, spreading of these three nerves. It exits from the orbital cavity above branches to the skin of the temporal region and the anterior the pulley of the superior oblique muscle, and supplies the part of the auricle [21–23]. The frontal branch, which is intermediate and outside the orbit, surrounds the orbital margin of the frontal bone and 8 First Visit and Patient Selection ascends to supply the skin of the frontal region. The supraorbital branch is the largest and most lateral of The first doctor-patient approach aims at giving both of them the branches of the frontal nerve. For the doctor it is important to evaluate the orbital foramen of the frontal bone along with the supraor- psychological aspects of the patient, determine the motiva- bital artery. Along its course it gives off numerous ascending tions behind the surgical operation, and discuss the possible branches that extend to the scalp. As a consequence, the surgeon must suggest ous branches for the forehead and the scalp, the supraorbital the best strategy without promising miraculous results. He nerve supplies the skin and the conjunctiva of the middle should rather find the best solution in every case, considering upper eyelid. During the inter- occipital nerve, is the largest posterior branch of the spinal view the patient can be accompanied by relatives or friends. It arises from between the first and second cervical Such company, in fact, facilitates a more serene and cordial vertebrae, and ascends medially and obliquely below the interview and puts the patient at ease. It then passes through the semispi- The questions can then be addressed to the accompanying nalis and trapezius muscles running subcutaneously in the person, and/or can be better explained and understood. During its initial course it gives branches important to plan the interview in different steps and sessions for the inferior oblique, semispinalis, longissimus capitis, in a cooperative and friendly ambience. It also spreads two collateral given should be quantitatively adequate for the patient. The dorsal ramus of cervical spinal nerve 3, outside the Therefore, they require less interview time than non-operated intervertebral foramen, runs backward toward the vertebral or poorly and badly informed patients. The interview will aim at informing the patient about the new medial branch runs upward medial to the greater occipital surgical methods and the more natural results that can be nerve, supplying the skin of the nuchal region. The lesser occipital nerve and the great auricular nerve The first visit, therefore, is a fundamental communicative originate from the cervical plexus. They pierce the superficial process through which the patient expresses his expectations cervical fascia posterior to the sternocleidomastoid muscle.
Generic 800 mg aciclovir free shipping. PHYSICAL CHANGES CAUSED BY MY HIV!.