Northern Illinois University. I. Lee, MD: "Buy cheap Levlen online no RX - Quality online Levlen".
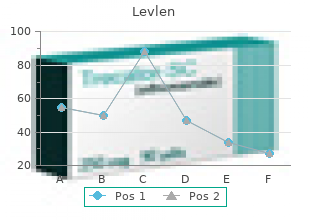
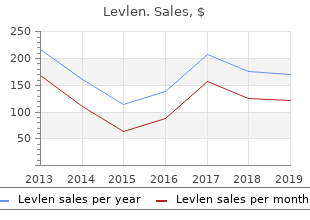
Acute therapy to terminate a tachycardia may be different from chronic therapy to prevent recurrence safe 0.15 mg levlen birth control for women cincinnati. Some of the exceptions are indicated in the footnotes; the reader is referred to text for a complete discussion cheap levlen 0.15 mg birth control for 3 years. The maximum heart rate achieved during strenuous physical activity varies widely but decreases with age cheap levlen 0.15mg birth control for women dresses. The P-P interval can vary slightly from cycle to cycle generic levlen 0.15 mg with amex birth control pills and periods, especially at slower rates, when the normal contour can develop a larger amplitude and become peaked. Accelerated phase 4 diastolic depolarization of sinus nodal cells (see Chapter 34) generally causes sinus tachycardia, usually from elevated adrenergic tone or withdrawal of parasympathetic tone. Carotid sinus massage and Valsalva or other vagal maneuvers gradually slow sinus tachycardia, which then accelerates to its previous rate on cessation of the enhanced vagal tone. More rapid sinus rates can fail to slow in response to a vagal maneuver, particularly those driven by high adrenergic tone. Clinical Features Sinus tachycardia is common in infancy and early childhood and is the normal reaction to various physiologic or pathophysiologic stresses, such as fever, hypotension, thyrotoxicosis, anemia, anxiety, exertion, hypovolemia, pulmonary emboli, myocardial ischemia, congestive heart failure, and shock. Atropine, catecholamines, and thyroid medications, as well as alcohol, nicotine, caffeine, and amphetamines or other stimulants, can produce sinus tachycardia. In patients with structural heart disease, sinus tachycardia can result in reduced cardiac output or angina or can precipitate another arrhythmia, in part related to the abbreviated ventricular filling time and compromised coronary blood flow. Chronic inappropriate sinus tachycardia (also known as the syndrome of inappropriate sinus tachycardia) has been described in otherwise healthy persons, possibly secondary to increased automaticity of the sinus node or an automatic 5 atrial focus near the sinus node. Both syndromes can result from autonomic neuropathy, either peripheral, as in diabetic patients, or central, from spinal cord injury. After three spontaneous sinus-initiated beats, premature stimulation of the high right atrium (S , S ) initiates a sustained tachycardia at a cycle length of 450 milliseconds that2 3 has the identical high-low atrial activation sequence characteristic of sinus node discharge. The most common reversible causes include hyperthyroidism, anemia, infection or inflammation, and hypovolemia. Elimination of tobacco, alcohol, caffeine, or other stimulants, such as the sympathomimetic agents in nose drops and cold medications, may be helpful. Beta blockers and nondihydropyridine calcium channel blockers (verapamil and diltiazem), fluid replacement in a hypovolemic patient, or fever reduction in a febrile patient can help slow the sinus nodal discharge rate. Treatment of inappropriate sinus tachycardia requires beta blockers or calcium channel blockers, alone or in combination. A specific blocker of the pacemaker current (I ), ivabradine, has been useful in somef patients with inappropriate or refractory sinus tachycardia. Premature Atrial Complexes Premature complexes are among the most common causes of an irregular pulse and palpitations. Premature complexes are common in normal hearts and increase in frequency with age. The contour of a premature P wave can resemble that of a normal sinus P wave, although it generally differs. Variations in the basic sinus rate can make the diagnosis of prematurity difficult, but differences in the contour of the P waves are usually apparent and indicate a different focus of origin. Reset (noncompensatory pause) occurs when the A -A1 2 interval plus the A -A interval is less than two times the A -A interval and the A -A interval is greater2 3 1 1 2 3 than the A -A interval. Often when this happens, the interval between the A and the next sinus-initiated P wave exceeds the A -A interval. In most cases, clear identification of the mechanism cannot be made clinically because the clinical and electrophysiologic features can overlap, especially when the reentrant circuit is small (i. Atrial Flutter and Other Macroreentrant Atrial Tachycardias Atrial flutter is the prototypic macroreentrant atrial rhythm. The typical atrial flutter is a reentrant rhythm in the right atrium that is constrained anteriorly by the tricuspid annulus and posteriorly by the crista terminalis and eustachian ridge. The flutter can circulate in a counterclockwise direction around the tricuspid annulus in the frontal plane (counterclockwise flutter) or in a clockwise direction (clockwise or reverse flutter). Rarely, intra-isthmus flutter can occur when the reentrant circuit is isolated to the cavotricuspid isthmus rather than rotating around the entire tricuspid annulus; this typically occurs after ablation in this region (usually done as treatment of typical flutter). Other forms of atrial flutter are now recognized as distinct types and include 7 atrial macroreentry caused by incisional scars from previous atrial surgery, previous atrial ablation, 8 mitral annular flutter, idiopathic fibrosis in areas of the atrium, or other anatomic or functional barriers to conduction in the atria. Because the barriers that constrain these flutters are variable, the electrocardiographic pattern of these atrial flutters can vary. Sometimes, flutter wave morphology changes during the same episode of flutter, which indicates multiple circuits or nonfixed conduction barriers. If such slowing occurs, the ventricles can respond in a 1 : 1 fashion to the slower atrial rate. During 2 : 1 or 1 : 1 conduction, transient slowing of the ventricular response with carotid sinus massage or adenosine is necessary to visualize the flutter waves. The flutter waves for the most common form, counterclockwise typical atrial flutter, are inverted (negative) in these leads because of a counterclockwise reentrant pathway, and sometimes they are upright (positive) when the reentrant loop is clockwise (see Fig. When the flutter waves are upright from clockwise rotation, they are often notched. The ratio of flutter waves to conducted ventricular complexes is most often an even number (e. However, these tachycardias frequently have a flutter rate similar to that of typical flutter (250 to 350 beats/min). After extensive left atrial ablation for atrial fibrillation, the electrocardiographic pattern of even typical flutter can change because of the altered left atrial activation caused by altered conduction secondary to ablation. This tachycardia uses a reentrant circuit established by the atriotomy on the lateral atrial wall. It can result from atrial dilation caused by septal defects, pulmonary emboli, mitral or tricuspid valve stenosis or regurgitation, heart failure, previous 10 extensive atrial ablation, and aging, but it can also occur without underlying heart disease. Toxic and metabolic conditions that affect the heart, such as thyrotoxicosis, alcoholism, and pericarditis, can cause atrial flutter. When it follows surgical repair of congenital heart disease, most patients can have both typical flutter and atypical flutter involving the atriotomy, often occurring years after the surgery. Carotid sinus massage usually decreases the ventricular rate in stepwise multiples; the ventricular rate returns in reverse manner to the former rate when carotid massage stops. Management Cardioversion is usually the initial treatment of choice for atrial flutter because it promptly and effectively restores sinus rhythm (see Chapter 36). Ibutilide appears to successfully cardiovert approximately 60% to 90% of episodes of atrial flutter. Other medications, such as procainamide or amiodarone, can be given to convert atrial flutter chemically, but they are generally less effective than ibutilide. Rapid atrial pacing with an esophageal or right atrial catheter can effectively terminate typical and some forms of atypical atrial flutter in most patients. Because catheter ablation is highly effective for typical flutter and because of the high relapse rate after cardioversion, catheter ablation is the preferred approach for stable patients who do not require immediate cardioversion. If calcium channel blockers and beta blockers in combination are insufficient, digoxin can be added. The dose of digitalis necessary to slow the ventricular response varies and at times can result in toxic levels because it is often difficult to slow the ventricular rate during atrial flutter. Side effects, especially proarrhythmic responses, must be carefully considered (see Chapter 36).
This provides additional scleral support that is especially helpful in children or patients who have undergone previous cataract surgery buy 0.15 mg levlen with mastercard birth control pills janelle. The donor corneal button is removed from the surrounding corneoscleral rim with a trephine and kept in storage medium until the recipient bed is prepared best 0.15mg levlen birth control for 3 years pregnancy. The host cornea is then trephined in a previously marked central location cheap levlen 0.15mg amex birth control question hotline, using either manual or vacuum-assist techniques while the anterior chamber is maintained with viscoelastics buy 0.15mg levlen overnight delivery birth control blood clots. After the eye is opened, it is critical to avoid patient movement, coughing, bucking, or any Valsalva maneuvers to prevent expulsion of the intraocular contents through the wound. The donor cornea is then sutured endothelial side down into place with 10-0 nylon sutures, which can be accomplished using 16 interrupted sutures (generally preferred with corneas that are inflamed, thinned, or vascularized), running sutures, or a combination, depending on a number of factors unique to each patient. Great care is taken during manipulation of the allograft to avoid trauma to the inner surface of the graft, as damage to the endothelial cells in this location can result in primary graft failure. Partial-thickness transplants, called lamellar keratoplasty, also can be performed in certain clinical situations. However, in patients with significant coagulopathy, a history of perforated corneal ulcers, severe systemic disease, or other conditions that make the use of these forms of anesthesia less preferable, corneal transplant can be performed with topical anesthesia in cooperative patients. It is the second most common cause of blindness in the United States and accounts for more than 5. In trabeculectomy, a drainage fistula (ostium) is created from the anterior chamber to the subconjunctival space, allowing aqueous humor to drain from the eye. First, a limbus-based or fornix-based incision is created in the conjunctiva and Tenon’s layer, exposing the underlying bare sclera. Because scarring (secondary to inflammation) is the most common cause of surgical failure, antimetabolites, such as mitomycin-C or 5-fluorouracil, are often applied to the surgical site to slow or prevent fibroblast proliferation. Next, an incision into the anterior chamber is created at the base of the scleral flap and converted to a sclerotomy by removing an approximate 1 × 4 mm piece of corneoscleral tissue. To prevent the iris from entering the ostium as well as to protect against future angle closure, an iridectomy is performed, followed by closure of the overlying scleral flap with 10-0 nylon sutures. Before closure, it is important to avoid coughing, bucking, or Valsalva maneuvers, which might cause suprachoroidal hemorrhage or expulsion of intraocular content. The conjunctiva is then reapposed, using running 8-0 or 9-0 absorbable or nylon sutures. These devices differ in implant size and whether or not there is an internal valve to prevent excessive drainage. Silicone tube is inserted into anterior chamber via needle track and is connected to a subconjunctival acrylic plate that is attached to the sclera near the equator. An alternative procedure is a trabeculotomy performed by exposing Schlemm’s canal (the drainage system) in a corneoscleral cutdown. A trabeculotome is then threaded into this canal and is rotated, creating a tear in the trabecular meshwork and allowing direct communication between the anterior chamber and Schlemm’s canal. Subconjunctival anesthesia at the bleb site may be associated with a poorer outcome, because it may stimulate fibroblasts to cause scarring due to hemorrhage and tissue damage. Peribulbar and retrobulbar injections in patients with advanced glaucoma may be associated with increased intraocular pressure, which can be prevented by decreasing anesthetic volumes and avoiding the use of orbital Honan balloons. Topical and intracameral anesthesia are being increasingly employed for trabeculectomy to avoid injection pain and potential complications, such as conjunctival button holes and hemorrhage. However, topical agents have the following limitations: inferior duration and intensity of anesthetic effect and lack of ocular akinesia, which is necessary to prevent globe compression in patients with prominent eyelid squeezing. Intracameral lidocaine as a supplement to topical anesthesia has the theoretical advantage of increasing depth of anterior chamber, but it poses the risk of damaging the phakic lens and excessive iridectomy enlargement. To avoid these possible complications, intracameral acetylcholine or topical pilocarpine can be used in conjunction with intracameral lidocaine. The surgical approach depends on the underlying anatomic abnormality, which can be congenital, involutional, cicatricial (scarring), or due to mechanical traction from masses or facial nerve palsy. A lateral tarsal strip procedure is often used, with the lateral canthal tendon first released by performing a lateral canthotomy and cantholysis of the crus (Fig. A lateral portion of tarsus is then dissected free of overlying skin, muscle, and conjunctiva. This strip of tarsus is trimmed to the appropriate length and is secured to the periosteum of the lateral orbital rim with suture. If punctal malposition is present, the tarsal strip procedure may be combined with a medial conjunctival spindle procedure. Alternatively, a full-thickness skin graft may be required and can be harvested from the upper lid or the postauricular or supraclavicular regions. The surgical approach depends on the underlying anatomic abnormality, which can be congenital, spastic, involutional, or cicatricial (scarring). For the more common involutional or age-related cases, the primary defect involves horizontal lid laxity, disinsertion of the lower lid retractors, and/or an overriding orbicularis muscle. Correction often involves use of the lateral tarsal strip procedure (see description under Ectropion Repair) to achieve tightening of the lower lid. Reattachment of the eyelid retractor muscles/aponeurosis may also be used in certain cases, either alone or in addition to a tarsal strip procedure. Variant procedure or approaches: Cicatricial entropion results from a contracting scar of the tarsus and/or conjunctiva pulling the lid margin inward. Correction requires release of this tension and either a lid-splitting procedure with tarsal advancement, rotational grafts, or free mucosal grafts harvested from hard palate. In the latter case, nasal intubation will be required to allow access to the graft site. Quickert procedure involves the placement of 2–3 sutures under local anesthesia to evert the eyelid. Causes include congenital maldevelopment, mechanical traction, myogenic conditions (e. The surgical approach depends primarily on the presence or absence of adequate levator muscle function that is responsible for elevating the upper eyelid. The most common etiology is age-related dehiscence or disinsertion of the levator aponeurosis from its normal attachment to the tarsus. Because levator muscle function is usually satisfactory in these patients, surgical correction involves reinserting the aponeurosis to the anterior tarsus alone or in combination with shortening of the aponeurosis by advancement or resection. Removal of excess skin and orbicularis muscle (blepharoplasty) may be performed simultaneously. Although several formulas have been devised to determine the amount of aponeurotic shortening, intraop measurement usually is performed to ensure that the appropriate lid position and contour are achieved. This requires that the procedure be performed under local anesthesia and that the patient be positioned and draped in a way that allows him/her to sit upright during surgery. Variant procedure or approaches: In patients with levator muscle function that is not adequate to achieve eyelid elevation, a frontalis sling procedure is performed to elevate the upper eyelid (Fig. More commonly required in children with congenital ptosis, this allows the patient to open the eye by elevating the brow. A variety of materials can be used to accomplish this suspension, including silicon rods or fascia. In children < 3 yr, autologous fascia lata can be harvested from the outer thigh from hip to knee. The material is tunneled beneath the skin and muscle from the brow incisions to the anterior tarsal region of the eyelid using Wright needles.
These patients generic levlen 0.15mg mastercard birth control zovia, almost all women discount levlen 0.15mg visa birth control arm implant, also show exaggerated sympathetic nervous system stimulation as indicated by markedly elevated plasma catecholamine levels buy levlen 0.15mg line birth control for women 8 weeks. Mental Stress A useful method of assessing the effects of stress and emotion on cardiac function is to measure transient ischemic responses to a standardized psychological stress challenge in the laboratory buy levlen 0.15 mg birth control spotting, or “mental stress test,” using mental arithmetic, color naming, public speeches, and similar tasks (see also Chapter 57). This methodology has the advantage of direct experimental manipulation where potential confounding factors can be controlled or eliminated and causal factors and their mechanisms directly investigated. However, this approach is necessarily limited to short-term responses to acute stress artificially induced in the laboratory, and thus may lack practical significance. In addition to cardiovascular reactivity, an important phenomenon that has been studied in conjunction with mental stress in cardiac patients is mental stress–induced myocardial ischemia. This condition is 11 analogous to exercise stress ischemia, except that the stimulus is psychological rather than physical. Mental stress ischemia has been studied with a variety of imaging techniques and a range of stressful 12,13 stimuli. The literature indicates that mental stress ischemia can be induced in one third to two thirds of coronary heart disease patients; younger women with coronary heart disease appear especially 14 susceptible. It is typically painless, and occurs at lower levels of oxygen demand than ischemia due to physical exertion. In addition, mental stress–induced ischemia is generally not related to the severity of coronary artery disease, suggesting that it is not simply a reflection of coronary disease severity. Patients may develop ischemia with mental stress but not with exercise or pharmacologic stress, although results vary. Ischemic responses are induced not only by severe emotional stress, but also by milder challenges similar to those that might be encountered in everyday life. In fact, mental stress–induced (but not exercise-induced) myocardial ischemia is correlated with ischemia measured in daily life ambulatory monitoring. Thus, mental stress testing could potentially provide a means for the identification of patients vulnerable to myocardial ischemia in everyday life. All the results published to date have indicated that mental stress–induced ischemia is a predictor of a poor prognosis. Five longitudinal studies with a follow-up of 1 to 5 years have found a consistent doubling of the risk of death or subsequent cardiac events. Although the samples of patients followed longitudinally to date are small, current evidence indicates that myocardial ischemic responses to standardized mental stress are prognostically important at least as much as responses to exercise- induced ischemia. Potential Mechanisms of Acute Stress as a Trigger of Cardiac Events A key pathophysiologic event underlying an acute coronary event is the progression from a stable plaque to a “vulnerable” plaque. No direct evidence exists to show that acute psychological stress causes atherosclerotic plaque rupture or erosion. However, acute episodes of stress or intense emotions may trigger acute coronary events in susceptible individuals by affecting plaque stability and disruption. This occurs through hemodynamic activation (increases in blood pressure and heart rate), increases in systemic vascular resistance, coronary vasoconstriction, inflammation, and prothrombotic effects, among others. Triggering usually takes place against a background of advanced atherosclerosis; thus it is considered 16 rare in people without underlying coronary artery disease. The mechanisms behind emotional triggering of acute myocardial ischemia, such as ischemia induced by mental stress, are likely multiple and may include hemodynamic changes, such as increases in blood pressure, heart rate, systemic vascular resistance, and coronary artery vasoconstriction. It is clear, however, that different hemodynamic responses underlie ischemia triggered by acute psychological stress 11,17 as compared with exercise stress. Myocardial ischemic responses to mental stress occur at a lower rate-pressure product than responses to exercise-induced ischemia in the same patients, although the hemodynamic response tends to be larger than in patients who do not become ischemic. Both people with and without preexisting coronary heart disease who develop mental stress ischemia show an increase in systemic vascular resistance, suggesting that a rise in afterload caused by peripheral vasoconstriction may 13 play a role in ischemia induced by psychological stress. Patients with atherosclerosis may undergo a paradoxical constriction during mental stress, particularly at points of stenosis, which may reduce myocardial blood flow and thus result in ischemia. Both coronary endothelial dysfunction and vasomotor abnormalities in the coronary microvasculature appear to play a role in myocardial ischemia triggered by psychological stress. Acute mental stress can also induce cardiac electrical instability, including an increase in T-wave alternans and other measures of abnormal cardiac repolarization that have been related to 18 arrhythmogenesis and sudden cardiac death (see also Chapter 34). Autonomic dysfunction and its effects on cardiac electrophysiology form another likely process underlying acute adverse effects of stress on the heart (see also Chapter 99). Both sympathetic activation and parasympathetic withdrawal can stimulate arrhythmias and lower the threshold for ventricular fibrillation. Heart rate variability, a measure of the beat-to-beat changes in heart rate as the heart responds to internal and external stimuli, is an accepted noninvasive measure of overall cardiac autonomic function (see also Chapter 12). Reduced heart rate variability predicts coronary heart disease in population studies, as well as death, particularly 19 sudden cardiac death, in patients following acute myocardial infarction. Heart rate variability is reduced during acute mental stress in the laboratory, and was found to be reduced during major disasters, such as earthquakes or terroristic attacks, in studies of patients who were undergoing ambulatory 1 electrocardiographic monitoring at the time of the event. These mechanisms may underlie the described connection of acute stress with life-threatening cardiac arrhythmias and sudden cardiac death. Inflammation and immunity are increasingly recognized as key factors in mediating cellular responses to acute psychological stress. Noradrenaline-dependent adrenergic stimulation due to stress activates the transcription factor nuclear factor κB in circulating monocytes, resulting in initiation of the inflammation cascade. Thus psychosocial stress stimulates mononuclear cell activation and subsequent immune and 20 inflammatory responses, which may result in myocardial ischemia. At the same time, stress-induced neuroimmune circuits involving microglia activation in the brain and sympathetic outflow to the 21 peripheral immune system further reinforce stress-related behaviors and the inflammatory phenotype. Thus, there are multiple physiologic responses secondary to emotional stress that could trigger cardiac ischemia or sudden death. However, presently little prospective information is available to link these mechanisms of acute stress to cardiovascular endpoints. Acute Stress and Cardiovascular Disease: Clinical Implications The clinical significance of acute emotional triggers of cardiac events has not been clearly established. Although the relative risk associated with acute stress is substantial, the absolute risk is smaller, given that these events are relatively uncommon. Furthermore, it is likely that this risk only affects a subset of vulnerable individuals. Some patients may be particularly susceptible to physiologic responses to emotional stimuli and therefore be at higher risk of unfavorable cardiovascular consequences due to stress. If such patients could be identified in advance, specific procedures could be put in place to minimize their exposure to an emotional trigger as well as reduce the risks associated with such exposure. Although it has been argued that programs that would increase awareness of psychological triggers among clinicians and the public would be beneficial, such programs in general lack evaluation. Chronic Stress Work Stress Work stress has been extensively studied for its potential adverse cardiovascular effects. A dominant 22 model of work stress includes the “job strain” model developed by Karasek and Theorell. The job strain model postulates that high work demands in combination with low control produce stress, because workers in low-control jobs cannot moderate work pressure by organizing their time or by other means. A third dimension of social support at work was later added, such that the adverse health effects of job stress are greatest in workers who lacked support from colleagues. An alternative model is the effort- reward imbalance model, which proposes that stress occurs when there is a mismatch between high workload and low payback in terms of money, job security, or other forms of recognition.
Purchase 0.15 mg levlen otc. MY SKIN AFTER THE PILL | 19 ways I healed my skin after stopping the pill.
Syndromes
- Medicine (dimercaprol or penicillamine) to reverse the effect of the poison
- Arterial blood gas
- The needle is removed.
- Treat the person for shock if he or she appears faint, pale, or if there is shallow, rapid breathing.
- Jaundice (yellow skin)
- Nausea
Pericarditis can be began to race quality levlen 0.15mg birth control for women 90s style, you felt faint levlen 0.15 mg line birth control libido, or you could not catch accompanied by fever generic levlen 0.15 mg line birth control pills to regulate hormones, rapid and shallow respirations buy levlen 0.15mg birth control essure, your breath? Panic Disorder In heart failure, decreased stroke volume reduces A response of “yes” to the above key questions can be the systolic blood pressure, and compensatory vaso- a highly sensitive screen for a psychogenic component constriction maintains a constant diastolic pressure. Patients with anxiety or depression often describe Pneumothorax is manifested by tachypnea and un- feelings of chest heaviness or tightness that can last equal chest wall excursion. In children, chest pain with tachycardia and hypoten- sion is generally caused by hypovolemia, secondary to a hemothorax, hemopneumothorax, or vascular injury. Observe for grimacing, area of chest pain for signs of the vesicular rash of diaphoresis, pallor, cyanosis, tachypnea, use of ac- herpes zoster. Petechial rash on the face and shoulders cessory muscles for breathing, splinting of chest can be a sign of protracted coughing as a result of wall, and unequal chest wall excursion. Tracheal shift can occur with pneumothorax and in People with fractured ribs or signifcant chest wall children with atelectasis, involving a signifcant por- contusions splint their chest wall, and take shallow tion of one lung. To assess the trachea for lateral dis- breaths to avoid aggravating pain with respiratory placement, position your index fnger frst on the right expansion. Abnormal trachea has shifted to the side, you will feel the wall on fndings for age can indicate chronic disease. In a pneumo- thorax, the trachea is deviated to the opposite side Measure Vital Signs and Note Respiratory Patterns during exhalation and toward the side of the pneu- Vital signs for people experiencing angina can be mothorax during inspiration. Hypotension can indicate cardiogenic Palpate the entire chest wall for tenderness, depres- shock. Fractured ribs and contusions will Chapter 8 • Chest Pain 87 result in tenderness to palpation and possible defor- Auscultate for Adventitious Sounds mity. Palpate each costochondral and chondrosternal Adventitious lung sounds are superimposed on normal junction. Costochondritis will be manifested by pain sounds and can be auscultated over any area of the lung with palpation over the cartilage between the sternum feld during inspiration or expiration. Palpation and range of joint motion can of abnormal lung sounds should include the type elicit arthritic pain in the shoulder or cervical spine. Rib pain on that increases peripheral airway resistance, obstructs the palpation in children without a reported history of peripheral airway, or causes a loss of elastic recoil will trauma can indicate child abuse. These indicate the presence of fuid, To check the chest wall for symmetry, frst test for mucus, or pus in the smaller airways. Fine crackles are diaphragmatic expansion of both the anterior and the soft and high pitched. Medium crackles are louder and posterior thorax between the eighth and tenth ribs. Each Wheezing is frequently described as a whistling thumb should move the same distance from the spine sound, and can be heard during inspiration, expira- or costal margins. Wheezing indicates that there is fuid in the large airways, such as in severe heart failure; more often it Percuss the Chest is associated with bronchospasm, as seen in asthma. Percussion in the area of pneumothorax will result in a Wheezing occurs on exhalation because that is when hyperresonant sound of an air-flled cavity. During inhalation, the nega- infltration, as in pneumonia, will produce a dull or fat tive pressure in the chest tends to hold open the air- sound. However, during exhalation, positive pressure in the alveoli is conducted from the outside of the Auscultate Breath Sounds small airways and tends to collapse them. The sound Instruct the patient to breathe through the mouth is usually polyphonic; this means that multiple, slowly and deeply. Auscultate systematically from the slightly different, high-pitched sounds are heard at lung apexes to the lower lobes anteriorly, posteriorly, the same time. If breath sounds are diminished over suggests a single area of blockage, such as with all lung felds, suspect chronic obstructive pulmonary a foreign body. Obese patients can have breath respiration is produced by intrathoracic airway sounds that are diffcult to auscultate. Breath sounds obstruction associated with lower respiratory tract will be inaudible in areas of pneumothorax. Palpate the abdomen for erated by turbulent air passing through secretions in tenderness and masses. Rhonchi can be present when the patient can occur with pancreatitis, esophagitis, or peptic ulcer has pneumonia. Cholelithiasis or cholecystitis can be mani- Pleural friction rub is a grating or squeaking sound fested by pain on palpation in the right upper quadrant. If abnormal lung sounds are detected, additional Examine the Extremities auscultation for bronchophony, egophony, and whis- Clubbing of the fngers can be an indication of chronic pered pectoriloquy are indicated (see Chapter 14). Peripheral cyanosis indicates hypoxia if accom- Auscultate Heart Sounds panied by central cyanosis. Consider exposure to a Auscultate for normal heart sounds in all positions, iden- cold environment, or anxiety, if peripheral cyanosis is tifying S , S , rate, and rhythm. Lower extremity edema is a sign of heart dial ischemia cannot be reliably performed by physical failure or venous stasis. Abnormal sounds, such as paradoxical S during2 sclerotic vessel disease or dissecting aortic aneurysm. A transient S (ventricular gallop) or mitral regur-3 gitation murmur at the apex can occur occasionally with Diagnostic tests are indicated when cardiovascular, myocardial ischemia or congestive heart failure. A summation gallop is the result of an S , S ,3 4 and rapid rate; this can also occur with heart failure. In children, ment elevation or depression indicates the presence of a loud murmur, best audible at the upper right sternal injured myocardium. T wave inversion demonstrates border, or upper left sternal border with a thrill, can the presence of ischemia. In aortic valve stenosis, a harsh ejection balance can also cause these variations from normal. Q systolic murmur, with radiation to the neck, is heard on waves are indicative of myocardial muscle loss but are auscultation. Midsystolic click/late systolic murmur (honk) is Evidence of ischemia is not always obvious on an heard with mitral valve prolapse. Observe the Spine for Evidence of Scoliosis People with scoliosis are at increased risk for pulmo- Stress Testing nary problems because of structural variations that can People experiencing intermittent chest pain who have cause compression of intrathoracic contents. Treadmill exercise testing uses a standard- movement or lack of movement of air in the lungs. An one of three categories: normal, high probability, and important objective of stress testing is to identify nondiagnostic. Radiographic contrast Exercise Myocardial Perfusion Imaging medium is injected into the pulmonary arteries, and the This imaging has greater accuracy than the standard vasculature is visualized. Radiography Pneumothorax and pneumonia can be identifed by Echocardiography chest radiography. Pneumothorax reveals evidence of An echocardiogram is a noninvasive cardiac ultra- pleural air, whereas pneumonia is seen on radiographs sound examining the heart that provides information as a parenchymal infltrate. It does not involve radiation and is used to sectional images of anatomical structures without su- differentiate healthy and diseased body tissues. It is useful in detecting abdomi- Ventilation-Perfusion Lung Scan nal aortic aneurysm and dissection, masses, fuid col- Ventilation-perfusion (V/Q) scanning was the frst line lections, and infection.