University of Hartford. Z. Ugolf, MD: "Buy cheap Metoprolol - Proven online Metoprolol OTC".
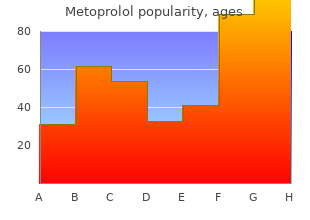
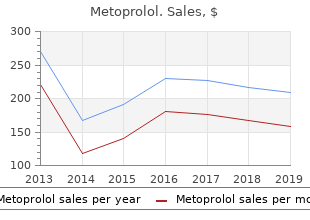
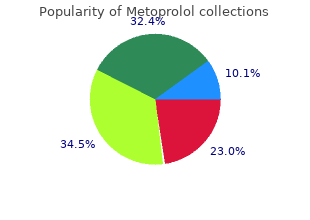
The right axillary artery is used for arterial return The suture line is sealed with a small amount of biological from the pump-oxygenator generic metoprolol 50 mg on-line blood pressure lowering medications. Afer the anastomosis artery using a 6-0 continuous polypropylene suture and is completed buy metoprolol 12.5mg without prescription pulse pressure folic acid, the aortic graf is clamped distal to the arch connected to the arterial line of the pump-oxygenator anastomosis and the graf is allowed to fill with blood buy metoprolol 50mg amex arrhythmia echocardiogram. A second arterial line from the pump-oxygenator is Afer establishing circulatory arrest using the tech- atached to the 10 mm side arm graf cheap 12.5mg metoprolol with amex pulse pressure 2013, and flow is initiated. Afer air has been evacuated from are freed from the surrounding tissue and transected at (a) (b) (c) (d) (e) (f) Figure 19. If necessary, they are divided more distally to avoid areas of atheroma or dissection. The clamp on the axillary artery graf is removed and perfusion is slowly initiated to evacuate entrapped air and debris (Figure 19. The brachiocephalic branches are gently clamped, and flow (10–15 ml/kg) at a tem- perature of 20–22°C is established to the brain by means of the axillary artery graf through the right carotid and right vertebral arteries. The flow rate is adjusted to maintain a mixed venous oxygen satura- tion (measured with a catheter in the right atrium) of 85–95%. In addition, oxygen saturation is monitored over both cerebral hemispheres, and perfusion pressure is monitored from the arterial pressure monitoring line in the lef arm. When the ing thoracic aorta, antegrade flow is established through the side arm of anastomoses are completed, the aortic graf is clamped the aortic graft as shown, or through an axillary artery graft, if present. The proximal end of the aortic graft is sutured to an existing ascending aortic distal to the lef subclavian artery, the clamps on the graft, or to a previously inserted or new aortic root-valve graft. Reproduced three branches are removed, and air is evacuated from with permission from [1]. The aortic graf is then clamped just proximal to the innominate artery, and antegrade flow is estab- lished through the three arteries from the axillary artery are performed. The proximal end of the aortic graf graf, while maintaining the same flow rate, pressure, and is sutured to the ascending aorta just above the level of temperature (Figure 19. Saphenous vein grafs, if present, are anas- to the distal aorta is completed at the appropriate level tomosed to the aortic graf with 5-0 or 6-0 polypropylene using an open technique and 3-0 or 4-0 polypropylene suture. The graf is stretched tightly from the heart and ascending aorta, and cardiopulmo- to avoid buckling. Those below this level, if patent, and, afer hemostasis has been achieved, the thoracotomy are preserved by beveling the aorta to maintain the pos- incision is closed afer placement of two drainage cath- terior wall or by ataching them to the aortic graf with eters in each pleural space. Hypothermic perfusion of the are also placed in the space between the pectoralis mus- brain is continued during this interval. Afer removal of the cannulae, the from the graf and the distal aorta by temporary release femoral artery and vein are repaired with 6-0 polypropyl- of the aortic clamp distal to the lef subclavian artery and ene suture. Flow to the lower body is then established in the antegrade direc- Patient selection tion from the axillary artery graf (Figure 19. Any remaining patent bronchial stage repair of the ascending aorta, the aortic arch, and or intercostal arteries are oversewn and the incised aortic varying lengths of the descending thoracic aorta using tissue is sutured around the aortic graf. The mean age of the During rewarming, aortic valve or aortic root replace- patients was 61 years (range 24–82 years), and 39 (70%) ment and coronary artery bypass grafing, if indicated, were men. Chronic ascending aortic dissection was the principal indication for use of this operative technique (Table 19. Of the 36 patients with this condition, 27 had undergone previous ascending aortic replacement, with or without Table 19. Of the remaining Arch perfusion (hypothemic) 34 ± 8 15–53 20 patients, 17 had extensive degenerative aneurysms, and Spinal cord and lower body ischemia 63 ± 15 20–90 3 had chronic descending dissections with proximal exten- Myocardial ischemia 145 ± 42 43–237 sion. Five of the 17 patients with degenerative aneurysms Rewarming 69 ± 15 35–110 Total cardiopulmonary bypass* 180 ± 47 103–290 had previous operations on the thoracic aorta. Perfusion data During the 10-year interval, patients with aortic dis- ease confined to the ascending aorta, the aortic arch, and Arterial return was established using a common femoral the first few centimeters of the descending thoracic aorta artery in 32 patients and the right axillary artery in 24 were operated upon through a median sternotomy [5]. The mean In two of these patients, a T-extension through the third durations of cooling, circulatory arrest, hypothermic intercostal space was required to facilitate exposure of the arch perfusion, spinal cord and lower body ischemia, descending thoracic aorta. Patients with aortic enlarge- myocardial ischemia, rewarming, and cardiopulmonary ment that extended below the diaphragm were managed bypass are shown in Table 19. For patients with aortic 50 minutes in 4 patients, and did not exceed 60 minutes dissection, the descending thoracic aorta was transected in any patient. Among the 21 patients in whom axillary at a level at which the diameter did not exceed 3–3. Reproduced with permission of hypothermic brain perfusion through the right carotid and right from [6]. During the latter period, oxygen saturation did not fall of hypothermic (20−22°C) perfusion of the brain from the of fresh frozen plasma, 5 units of platelets, and 9 units of right vertebral and right carotid arteries that averaged 30 ± cryoprecipitate. Inotropic support with more than 5 µg/kg/min of dob- Results utamine for more than 24 hours was required in 7 (13%) of the 55 operative survivors. Two patients required intra- operative insertion of a right ventricular assist device Early (hospital) death for right ventricular dysfunction. The device was removed on the third 71-year-old woman with a chronic expanding ascending post-operative day in the second patient, who had a full aortic dissection and severe aortic regurgitation afer a cor- recovery and was discharged from the hospital. Two of these aortic root replacement, and coronary artery bypass graf- patients died in the hospital. The other three patients died on the fifh, eighth, and had blood urea nitrogen and creatinine levels return to twenty-third post-operative days of multiple organ system baseline levels before discharge from the hospital. This technique patient, also with Marfan syndrome, required laparatomy continues to be widely used, particularly in combination for intraperitoneal bleeding resulting from spontaneous with the elephant trunk modification [10,11]. The mean dura- rience of Crawford and colleagues, perioperative stroke tion of post-operative hospital stay was 22 days (median with a focal neurological deficit was shown to be related 14 days; range 5–118 days). Late death Furthermore, because the duration of hypothermic circu- During the follow-up interval, which extends to latory arrest and increasing age are important predictors 88 months, there have been 9 late deaths. In our initial 35 patients, in whom a cuff of aorta surrounding the brachiocephalic arteries was sutured to the aortic graf, the duration of circulatory arrest aver- Late reoperations aged 39 minutes and did not exceed 60 minutes in any Four patients have undergone successful reoperations that patient. In the more recent 21 patients – using axillary involved the aortic graf (2 patients) or the remaining aorta artery cannulation for arterial return, a branched graf, (2 patients). One of these patients required reoperation on and an interval of hypothermic brain perfusion from the aortic root and the ascending aortic graf for presumed the right carotid and right vertebral arteries, during infection 15 months post-operatively. The aortic root was which the three brachiocephalic arteries were atached replaced with an aortic allograf, and the ascending por- to the branches of the aortic graf – the mean duration tion of the previously inserted aortic graf was replaced of circulatory arrest was reduced to 10 minutes and with a new polyester graf. At operation, erosion of the graf result- nique and in 5% of the patients with the branched graf ing from compression against a rib was noted, and a seg- technique, suggesting that this is a highly effective tech- ment of the graf was replaced. The arch first technique has a chronic descending aortic dissection, required replace- the additional advantages of providing arterial brain ment of the remaining contiguous thoracic and upper perfusion without the need for direct cannulation of the abdominal aorta for aneurysmal enlargement 34 months brachiocephalic arteries (a potential cause of emboliza- afer the initial operation. The fourth patient required tion and stroke), or for a separate perfusion circuit for resection of a separate infradiaphragmatic degenera- the brain.
The meninges are the site of subarachnoid hemorrhages proven 12.5mg metoprolol hypertension values, subdural and epidural hematomas buy cheap metoprolol 12.5 mg line blood pressure chart dot, meningitis metoprolol 100mg free shipping arrhythmia dance company, and hydrocephalus order 25 mg metoprolol amex prehypertension american heart association. The cerebral arteries are the site of cerebral hemorrhages, thrombosis, and emboli, as well as aneurysms and arteriovenous anomalies. The cerebral veins, especially the venous sinuses, may become inflamed and thrombosed, producing a headache. The cranial nerves are the site of trigeminal neuralgia mentioned above and glossopharyngeal neuralgia. Although the brain itself is not tender, lesions of the brain cause increased intracranial pressure or traction on other painful structures, such as the intracranial arteries, venous sinuses, or nerves. Concussions, pituitary tumors, toxic encephalopathy from alcohol, bromides, and other substances are important causes, in addition to the cerebral hemorrhage, thrombosis, and emboli already mentioned. The various systemic diseases shown in Table 33 are too numerous to mention here, but fever of any etiology is an important cause and must not be forgotten, although this symptom is usually obvious. If one approaches the challenge simply on the basis of what is common, the patient most likely has migraine or muscle traction headache. Shouldn’t we look for serious conditions such as brain tumor, meningitis, or subarachnoid hemorrhage to avoid a serious mistake and a malpractice suit? First, check for nuchal rigidity to rule out meningitis and subarachnoid hemorrhage. Next, do a careful neurologic examination to rule out a brain tumor or other space-occupying lesion. These steps are particularly important in a patient who is experiencing his or her first serious headache. If there is nuchal rigidity or focal neurologic signs, it is wise to immediately refer the patient to a neurologist or neurosurgeon for further workup and possible hospitalization. One other condition that must be considered in acute headache (particularly in elderly persons) is temporal arteritis. A sedimentation rate will usually be positive, but a neurology consult is axiomatic so that steroids can be started immediately. In the patient with chronic or recurring headaches and no neurologic findings, it is wise to see the patient during the attack. Migraine and histamine headaches can be diagnosed by the response to sumatriptan by mouth or injection. If the headaches are due to chronic allergic or infectious rhinitis, relief can be had by spraying the turbinates with phenylephrine. Muscle traction headaches will often be relieved by occipital nerve blocks supporting the diagnosis. Compression of the superficial temporal artery will often relieve migraine temporarily supporting that diagnosis. Compression of the jugular veins will often give relief to patients with postspinal tap headaches. If the patient is seen between headaches, certain prophylactic measures may help establish the diagnosis. For migraine, β-blockers may be prescribed; if the headaches are prevented, there is good support for the diagnosis. A course of corticosteroids may be initiated in patients with histamine (cluster) headaches to help establish the diagnosis. Muscle relaxants and/or tricyclic drugs may be given to help diagnose muscle contraction headaches. She was seen in the emergency room the night before and was diagnosed with migraine, given a shot, and sent home. On examination, the patient was found to have nuchal rigidity but no focal neurologic signs. I—Infection recalls syphilis in which the head assumes the shape of a hot cross bun. N—Neurologic disease includes microcephaly (small underdeveloped brain) and hydrocephaly (due to several causes); the most important diseases from a treatable standpoint are subdural hematomas, brain abscesses, and neoplasms. D—Deficiency disease suggests rickets, in which the head is elongated, 416 square, and flattened at the vertex. There is symmetric enlargement (occasionally a triangular shape) because the bones of the face do not enlarge. C—Congenital disorders include scaphocephaly (elongated from front to back), oxycephaly or tower skull, hypertelorism (increased breadth of the skull and eyes far apart), mongolism, and brachycephaly. T—Trauma recalls injury to the skull, causing edema (caput succedaneum), hematomas, and fractures. E—Endocrine disorders such as acromegaly, myxedema, and cretinism cause a large head. Approach to the Diagnosis Obviously, the most important thing in the workup of this symptom is a good neurologic examination and a skull x-ray film. Positional head deformity is most commonly caused by a child sleeping frequently in the supine position. An extensive discussion of skin masses may be found on page 381, but most head masses originating from the skin are sebaceous cysts, carbuncles, or 417 lipomas. Lesions of the skull that may present as focal lesions are metastatic tumors, multiple myeloma, osteitis fibrosa cystica (hyperparathyroidism), and osteomas. Brain tumors, subdural hematomas, and epidural abscesses may cause proliferation of the bone over the lesion and produce a mass. Congenital meningoceles and meningoencephaloceles may protrude through defects in the skull, producing large focal lesions in the midline. There are other causes, however, and the problem for the diagnostician is how best to recall these in the clinical situation. From an etiologic standpoint inflammation is almost invariably the culprit, although myocardial infarction or angina pectoris are two frequent causes that are not inflammatory. Anatomically, the best approach is to move in a target-like fashion from the intrinsic portion of the esophagus and stomach peripherally. Thus, in the first zone, one encounters esophagitis, gastritis, and gastric ulcers. In the second zone, one encounters hiatal hernia (which, of course, predisposes to esophagitis), pericarditis, mediastinitis, and gastrojejunostomy complications. In the third zone, one visualizes cholecystitis (which probably induces a bile esophagitis), pancreatitis, myocardial infarction or coronary insufficiency, pleurisy, and intestinal obstruction. If the patient has the pain when in your office, administer a tablespoon or two of lidocaine (Xylocaine viscous). If the patient gets relief in 5 to 10 minutes, the heartburn is probably caused by esophagitis. Esophagoscopy and gastroscopy will reveal most intrinsic lesions with certainty, but occasionally they are normal in esophagitis. Manometric studies of the esophagus are the best way to diagnose esophageal reflux. If the episodes are frequent but relatively brief, a trial of nitroglycerin may diagnose angina pectoris.
Gingivitis as part of a diffuse stomatitis may be seen in pemphigus discount 100mg metoprolol visa blood pressure medication lotrel, 582 Stevens–Johnson syndrome generic metoprolol 100mg online hypertension silent killer, Vincent stomatitis (spirilla and bacilli fusiformis) discount metoprolol 25 mg on-line heart attack symptoms, and various other bacterial forms buy metoprolol 50mg low cost arteria inflamada del corazon. The job of the clinician is to exclude the systemic causes and then refer the patient to a periodontist for evaluation and treatment of the local causes. Bleeding from the breast, hemorrhagic discharge: Suspect a neoplasm, such as a ductal carcinoma (Paget disease), fibroadenosis, and ductal papillomas, unless proven otherwise. With a magnifying glass, one may be able to tell which of the 20 or so ducts is bleeding, but expressing one small segment at a time, working spirally, is also helpful. Following the nerve impulse from the cerebral cortex down through the spinal cord, nerve roots, brachial and lumbosacral plexus, peripheral nerve, myoneural junction, and muscles allows us to recall the most significant causes of monoplegia. Cerebral cortex: Monoplegia may result from a parasagittal tumor or abscess and anterior cerebral artery embolism or thrombosis. Occasionally an occlusion of the middle cerebral artery or its branches may cause monoplegia of the upper extremity, but there are almost always neurologic signs in the lower extremities in these cases. Spinal cord: Early space-occupying lesions of the spinal cord and amyotrophic lateral sclerosis may present with monoplegia. Nerve roots: Poliomyelitis, progressive muscular atrophy, and herniated discs may present with monoplegia. Brachial plexus: This would bring to mind brachial plexus neuropathy, thoracic outlet syndrome, and Pancoast tumors. Peripheral nerve: Trauma or entrapment of the peripheral nerves may present as a monoplegia. Myoneural junction: Myasthenia gravis or Eaton–Lambert syndrome may occasionally present as weakness in one extremity. Muscle: It is unusual for the various forms of muscular dystrophy and dermatomyositis to present with monoplegia. Approach to the Diagnosis 583 The neurologic examination will help determine the site of the lesion and thus the likely etiology. If there are hyperactive reflexes in the involved extremity, the lesion is probably in the upper spinal cord or cerebral cortex. If there is associated facial palsy or other cranial nerve signs, the lesion is probably in the brain or brainstem. Hypoactive reflexes in the involved extremity indicate a lesion in the nerve roots, nerve plexus, or peripheral nerves. However, acute cerebral thrombosis, hemorrhage, or embolism may present with hypoactive reflexes in the involved extremity. Blood lead levels, glucose tolerance tests, and other studies indicated in a neuropathy workup (page 334) may be required. M—Malformation would bring to mind familial intestinal polyposis (Peutz–Jeghers syndrome) and Fabry disease. I—Inflammation would suggest the pigmentation of the buccal mucosa seen in pulmonary tuberculosis of the adrenal gland leading to Addison disease. N—Neoplasm suggests the pigmentation seen in metastatic malignant melanoma and carcinomatosis. T—Toxic helps recall the toxic substances that cause mouth pigmentation such as silver, bismuth, contraceptives, tranquilizers, antimalarials, lead, arsenic, and mercury. S—Systemic diseases associated with mouth pigmentation include Addison disease, hemochromatosis, and porphyria. Approach to the Diagnosis 584 If lead or arsenic poisoning is suspected, hair analysis may be done. If Addison disease is suspected, serum cortisol or a 24-hour urine 17- hydroxysteroids and 17-ketosteroids should be done. Certainly, the low-grade systolic murmurs tend to be functional; if the murmur changes or disappears on position, inspiration, or exercise it is likely to be functional. After the murmur is determined to be organic, one needs to have a working differential diagnosis in mind to proceed efficiently. N—Neoplasm includes atrial myxomas, the most significant disorder to remember here, but leukemic infiltration of the heart and all the neoplasms associated with anemia might be considered. D—Degenerative disease recalls atherosclerotic heart disease, muscular dystrophy, and Friedreich ataxia. Atherosclerotic heart disease should be emphasized because it frequently causes aortic murmurs. I—Intoxication reminds one that there may be no murmur in alcoholic 585 myocardiopathy until failure develops, but it is a condition to consider nevertheless. I—Idiopathic disorders include mitral valve prolapse, although in some cases this is hereditary. A—Autoimmune disease includes rheumatic fever, the best known of these disorders, although it is now a less frequent consideration in murmurs. T—Traumatic disorders recall a ventricular or aortic aneurysm and occasionally a coronary arteriovenous fistula or valvular insufficiency that may result from a stab wound. Hyperthyroidism produces murmurs in some cases because of the rushing blood and rapid rate, causing many eddy currents. Referral to a cardiologist is wise if the cause is obscure or if one is unable to spend the time for a careful workup. Angiocardiography and cardiac catheterization are the only sure ways to determine the location of the valvular disease, and, in many cases, the exact cause. Spinal cord disease When recalling the differential diagnosis of muscular atrophy, think of these seven factors and the causes will unfold. Lack of use of the muscle: In focal or generalized bone or joint disease there is diminished use of the extremity or part involved, so the muscles atrophy. Primary muscle disease: Muscular dystrophy, dermatomyositis, trichinosis, and McArdle syndrome should be considered here. Peripheral nerve disease: Diabetic neuropathy and the neuropathy from lead, arsenic, and other toxins should be considered here. Hereditary neuropathies such as Charcot–Marie–Tooth disease and Dejerine–Sottas hereditary hypertrophic neuritis are also considered here. Nerve root disease: Spinal column disorders that compress the root include fractures, herniated disks, spondylolisthesis, tuberculosis, metastatic tumors, and multiple myelomas. Spinal cord disease: The degenerative diseases such as amyotrophic lateral sclerosis, progressive muscular atrophy, and syringomyelia must be considered here. In addition, poliomyelitis, transverse myelitis of various areas, anterior spinal artery occlusion, infectious polyneuritis, and spinal cord tumors must be recalled. Approach to the Diagnosis Focal atrophy of a muscle often means a damaged peripheral nerve or root. If there are visible fasciculations, a lesion of the spinal cord or root is most likely. Muscle biopsy is valuable in ruling out trichinosis, dermatomyositis, or muscular dystrophy.
Buy 50mg metoprolol fast delivery. how to measure Blood pressure - Blood pressure measurement-learn bp.