Medical College of Georgia. P. Grimboll, MD: "Buy Escitalopram online in USA - Cheap Escitalopram OTC".
Decreased temperature and shivering can elevate oxygen consumption and escitalopram 5 mg low cost anxiety games, in some patients order escitalopram 10 mg with amex anxiety supplements, lower PaO [2 171 discount 20mg escitalopram overnight delivery anxiety symptoms following surgery,180] cheap 5 mg escitalopram otc anxiety after eating. Increased perioperative cardiac ischemia, ventricular tachycardia [181], delayed wound healing [106], perioperative bleeding requiring transfusion [107,182,183], increased length of stay in recovery, and increased length of stay in hospital [106] may occur with perioperative hypothermia. Patients with prolonged postoperative hypothermia have a higher mortality than those who return to normal temperatures in the first postoperative hour [184]. Prevention and Treatment Numerous interventions have been attempted to minimize perioperative temperature decrease and shivering. The use of postoperative warming blankets alone does not prevent significant temperature loss because the body surface area exposed to heat is small [18,174,185]. The use of warming blankets along with heating of all infused liquids can maintain average temperature on arrival in the recovery room above 36°C [185]. The inhalation of heated, humidified air can be safely applied to most intubated patients and is effective for preventing temperature loss [180,188,189] and shivering [180]. Most publications clearly favor the use of preoperative, intraoperative, and postoperative forced air warmers [190–192]. One hour of prewarming with an air warmer set to 43°C may minimize redistribution loss and decrease hypothermia for brief procedures. Vasodilators such as nitroprusside or nifedipine may be started hours preoperatively, resulting in peripheral vasodilation and minimizing redistribution loss by prewarming the peripheral tissues. Prevention of the development of hypothermia in summary includes minimizing preoperative and postoperative time in chilled rooms, covering the patient with drapes or blankets whenever possible, and infusing all solutions at least at room temperature. High-risk patients including those undergoing major abdominal or cardiothoracic surgery, surgery involving intentional hypothermia, or surgery with anesthesia times in excess of 4 hours; patients older than 60 years undergoing surgery; or those with known or expected cardiac depression should receive preventive measures, including preoperative [193–195] and intraoperative [191,196] forced warm air, heating of infused solutions to 37. In any patient undergoing extracorporeal bypass, a heat exchanger to the bypass circuit should be used [197]. Currently, mild-to-moderate hypothermia (32°C to 36°C) is the first treatment with proven efficacy for postischemic neurologic injury, and employing intentional hypothermia to retard postcardiac arrest brain injury is now recommended by the American Heart Association [226,220]. Therapeutic Hypothermia After Cardiac Arrest Therapeutic hypothermia improves survival and neurologic outcomes after sudden cardiac arrest, and has been summarized in a systematic review and meta-analysis of six randomized trials including 1,413 patients [199–201,225]. According to this review, patients treated with therapeutic hypothermia were more likely to survive than patients whose temperature was not managed similarly (relative risk: 1. Conclusion about the absence of any difference of outcomes based on the target temperature is based primarily on the findings of a large, well-performed, multinational randomized trial of 939 unconscious survivors of out-of-hospital cardiac arrest that reported no differences of mortality or neurologic function between patient’s treated with a target temperature of 33°C (n = 473) compared to patients with a targeted temperature of 36°C (n = 466) [220]. Cardiac arrest results in immediate termination of blood flow and loss of oxygen, leading to neurologic ischemic injury after only several minutes and permanent loss after 5 to 10 minutes. Several animal models, including dogs, showed that cooling after prolonged cardiac arrest provided considerable neurologic benefits [203]. Subsequently, two pivotal, randomized, controlled trials were conducted and confirmed efficacy [200,201]. The first of these was a large, multicenter, randomized controlled trial that enrolled 275 patients in 9 European hospitals who had sustained a cardiac arrest with an initial rhythm of ventricular fibrillation. The second randomized controlled trial enrolled 77 patients from 4 hospitals in Victoria, Australia, with similar inclusion criteria, however, did not exclude older patients or those who were hypoxic. The American Heart Association recommended, in review of these two studies, therapeutic hypothermia for 12 to 24 hours following resuscitation from out-of-hospital cardiac arrest for the treatment of neurologic injury when the initial rhythm is ventricular fibrillation [204]. Nonetheless, evidentiary support for therapeutic hypothermia in nonshockable rhythms is primarily limited to nonrandomized studies using historic or concurrent controls [205]. One subgroup analysis of 186 patients with a nonshockable rhythm reported no difference in mortality between those treated with temperature management using a target of 33°C versus a target of 36°C [220]. In addition, the trials used therapeutic hypothermia several hours after resuscitation; therefore, the role for earlier cooling or prolonged cooling was not evaluated. In a Cochrane database systematic review, when combined with standard postcardiac arrest care, lowering the body temperature to the range of 32°C to 34°C during the first hours after cardiac arrest improves neurologic outcomes compared to not controlling body temperature [219]. A large randomized trial reports similar improvements in outcome whether the temperature is maintained at 33°C or 36°C [220]. Given that the induction of hypothermia has become more feasible, the side effects are generally easily managed in the critical care setting, and there is a benefit for anoxic brain injury; consideration may be given to treat comatose postcardiac arrest nonventricular fibrillation patients with therapeutic hypothermia [205]. Failure to control a patient’s core temperature is associated with the development of fever and worse neurologic outcomes [221,222]. According to an observational study of 151 patients, the risk of death increases for each degree over 37°C during the first 48 hours after cardiac arrest (odds ratio: 2. Earlier onset of fever is associated with worse outcomes, whereas delayed fever onset has not shown the same deleterious effects [222]. Overall, these data suggest that active control of the postcardiac arrest patient’s core temperature, with a target between 32°C and 36°C, followed by active avoidance of fever, is the optimal strategy to promote patient’s survival. Although mild hypothermia appears feasible and safe, its ability to limit infarct size or reduce rates of adverse cardiac events has not been proven [206]. Hypothermia remains an experimental treatment with unknown clinical relevance for patients with acute spinal cord injury [207]. For Acute Liver Toxicity Patients with rapidly progressive acute liver failure, such as with acetaminophen overdose, are at high risk for developing cerebral edema, intracranial hypertension, brainstem herniation, brain death or anoxic brain injury, and permanent brain impairment. Techniques such as manipulating the body position, increasing sedation, and increasing osmolarity through medications can temporarily control this phenomenon. However, these steps often postpone but do not stop the development of brain herniation unless liver transplantation or spontaneous liver regeneration follows immediately. Using therapeutic hypothermia has been shown to effectively bridge patients to transplant by reducing cerebral edema and intracranial hypertension by decreasing splanchnic ammonia production, lowering oxidative metabolism within the brain, and restoring normal regulation of cerebral hemodynamics [209]. However, hypothermia has not been adequately studied for its safety, and concerns of increasing the risk of infection, cardiac arrhythmias, and bleeding may be accentuated. Multicenter, randomized control trials are needed to determine whether hypothermia protects the brain and improves survival without causing harm. In Multisystem Trauma Hypothermia may be helpful in attenuating the damage to tissues before adequate blood volume resuscitation can be restored in traumatic blood loss. Advances in hypothermia, based on randomized controlled trials or meta-analyses of such trials, are summarized in Table 184. Methods of Cooling Induction and maintenance of hypothermia requires blocking the body’s normal thermoregulation mechanism as well as active heat exchange. Therapeutic hypothermia can be achieved through four mechanisms individually or in combination, which include conduction, convection, radiation, and evaporation as previously described. There are four phases of temperature modulation during therapeutic hypothermia: induction, maintenance, rewarming, and normothermia [211]. In cardiac arrest survivors, contraindications to perform therapeutic hypothermia would include if the patient can follow verbal commands, more than 8 hours have elapsed since return of spontaneous circulation, life-threatening bleeding or infection, cardiopulmonary collapse is imminent despite vasopressor or mechanical hemodynamic support, or an underlying terminal condition exists. Simultaneous sedation, paralysis (for shivering), and use of commercial surface or intravascular cooling devices are concomitant therapeutic strategies [211]. Maintenance phase occurs in the intensive care unit and is a phase where both metabolic and hemodynamic homeostasis are maintained.
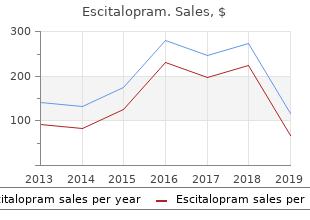
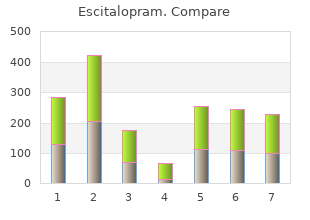
Etiology of Hypertension Although hypertension may occur secondary to other disease processes order 5 mg escitalopram overnight delivery anxiety symptoms ringing ears, more than 90% of patients have essential hypertension (hypertension with no identifiable cause) order escitalopram 20mg with amex anxiety guidelines. A family history of hypertension increases the likelihood that an individual will develop hypertension discount escitalopram 5mg amex anxiety fear. The prevalence of hypertension increases with age but decreases with education and income level proven escitalopram 5mg anxiety symptoms 6 weeks. Non-Hispanic blacks have a higher incidence of hypertension than do both non- Hispanic whites and Hispanic whites. Persons with diabetes, obesity, or disability status are all more likely to have hypertension than those without these conditions. In addition, environmental factors, such as a stressful lifestyle, high dietary intake of sodium, and smoking, may further predispose an individual to hypertension. Mechanisms for Controlling Blood Pressure Arterial blood pressure is regulated within a narrow range to provide adequate perfusion of the tissues without causing damage to the vascular system, particularly the arterial intima (endothelium). Arterial blood pressure is directly proportional to cardiac output and peripheral vascular resistance (ure 16. Cardiac output and peripheral resistance, in turn, are controlled mainly by two overlapping mechanisms: the baroreflexes and the renin– angiotensin–aldosterone system (ure 16. Most antihypertensive drugs lower blood pressure by reducing cardiac output and/or decreasing peripheral resistance. Baroreceptors and the sympathetic nervous system Baroreflexes act by changing the activity of the sympathetic and parasympathetic nervous system. Therefore, they are responsible for the rapid, moment-to-moment regulation of blood pressure. A fall in blood pressure causes pressure-sensitive neurons (baroreceptors in the aortic arch and carotid sinuses) to send fewer impulses to cardiovascular centers in the spinal cord. This prompts a reflex response of increased sympathetic and decreased parasympathetic output to the heart and vasculature, resulting in vasoconstriction and increased cardiac output. Renin–angiotensin–aldosterone system the kidney provides long-term control of blood pressure by altering the blood volume. Baroreceptors in the kidney respond to reduced arterial pressure (and to sympathetic stimulation of β -adrenoceptors) by releasing the enzyme1 renin (ure 16. Treatment Strategies the goal of antihypertensive therapy is to reduce cardiovascular and renal morbidity and mortality. For most patients, the blood pressure goal when treating hypertension is a systolic blood pressure of less than 130 mm Hg and a diastolic blood pressure of less than 80 mm Hg. However, initial drug therapy choice may vary depending on the guideline and concomitant diseases (ure 16. If blood pressure is inadequately controlled, a second drug should be added, with the selection based on minimizing the adverse effects of the combined regimen and achieving goal blood pressure. Patients with systolic blood pressure greater than 20 mm Hg above goal or diastolic blood pressure more than 10 mm Hg above goal should be started on two antihypertensives simultaneously. Combination therapy with separate agents or a fixed-dose combination pill may lower blood pressure more quickly with minimal adverse effects. A variety of combination formulations of the various pharmacologic classes are available to increase ease of patient adherence to treatment regimens that require multiple medications. Individualized care Hypertension may coexist with other conditions that can be aggravated by some of the antihypertensive drugs or that may benefit from the use of some antihypertensive drugs independent of blood pressure control. In such cases, it is important to match antihypertensive drugs to the particular patient. In addition to the choice of therapy, blood pressure goals may also be individualized based on concurrent disease states and age (ure 16. Diuretics For all classes of diuretics, the initial mechanism of action is based upon decreasing blood volume, which ultimately leads to decreased blood pressure. Routine serum electrolyte monitoring should be done for all patients receiving diuretics. A complete discussion of the actions, therapeutic uses, pharmacokinetics, and adverse effects of diuretics can be found in Chapter 17. This causes a decrease in extracellular volume, resulting in a decrease in cardiac output and renal blood flow (ure 16. With long-term treatment, plasma volume approaches a normal value, but a hypotensive effect persists that is related to a decrease in peripheral resistance. Thiazide diuretics can be used as initial drug therapy for hypertension unless there are compelling reasons to choose another agent. Thiazide diuretics can induce hypokalemia, hyperuricemia, and, to a lesser extent, hyperglycemia in some patients. Loop diuretics the loop diuretics (furosemide, torsemide, bumetanide, and ethacrynic acid; see Chapter 17) act promptly by blocking sodium and chloride reabsorption in the kidneys, even in patients with poor renal function or those who have not responded to thiazide diuretics. Loop diuretics cause decreased renal vascular resistance and increased renal blood flow. However, unlike thiazides, loop diuretics increase the calcium content of urine, whereas thiazide diuretics decrease it. These agents are rarely used alone to treat hypertension, but they are commonly used to manage symptoms of heart failure and edema. Aldosterone antagonists have the additional benefit of diminishing the cardiac remodeling that occurs in heart failure (see Chapter 18). Potassium-sparing diuretics are sometimes used in combination with loop diuretics and thiazides to reduce the amount of potassium loss induced by these diuretics. Actions the β-blockers reduce blood pressure primarily by decreasing cardiac output (ure 16. The selective β-blockers may be administered cautiously to hypertensive patients who also have asthma. The nonselective β-blockers are contraindicated in patients with asthma due to their blockade of β -2 mediated bronchodilation. Therapeutic uses the primary therapeutic benefits of β-blockers are seen in hypertensive patients with concomitant heart disease, such as supraventricular tachyarrhythmia (for example, atrial fibrillation), previous myocardial infarction, stable ischemic heart disease, and chronic heart failure. Conditions that discourage the use of β-blockers include reversible bronchospastic disease such as asthma, second- and third-degree heart block, and severe peripheral vascular disease. Pharmacokinetics the β-blockers are orally active for the treatment of hypertension. The β-blockers may decrease libido and cause erectile dysfunction, which can severely reduce patient compliance. Alterations in serum lipid patterns Noncardioselective β-blockers may disturb lipid metabolism, decreasing high-density lipoprotein cholesterol and increasing triglycerides. Drug withdrawal Abrupt withdrawal may induce severe hypertension, angina, myocardial infarction, and even sudden death in patients with ischemic heart disease.
Bisphosphonates are rapidly cleared from the plasma buy escitalopram 10 mg free shipping anxiety zen, primarily because they avidly bind to hydroxyapatite in the bone buy escitalopram 20 mg anxiety 40 weeks pregnant. Elimination is predominantly via the kidney cheap 5 mg escitalopram anxiety brain, and bisphosphonates should be avoided in severe renal impairment cheap escitalopram 10 mg on-line anxiety research. For patients unable to tolerate oral bisphosphonates, intravenous ibandronate and zoledronic acid are alternatives. Alendronate, risedronate, and ibandronate are associated with esophagitis and esophageal ulcers. To minimize esophageal irritation, patients should remain upright after taking oral bisphosphonates. Although uncommon, osteonecrosis of the jaw and atypical femur fractures may occur with use of bisphosphonates. The risk of atypical fractures seems to increase with long-term use of bisphosphonates. Therefore, current guidelines recommend a drug holiday for some patients after 5 years of oral bisphosphonates or 3 years of zoledronic acid. Denosumab is approved for the treatment of postmenopausal osteoporosis in women at high risk of fracture. Denosumab is considered a first-line agent for osteoporosis, particularly in patients at higher risk of fractures. The drug has been associated with an increased risk of infections, dermatological reactions, hypocalcemia, and rarely, osteonecrosis of the jaw, and atypical fractures. These drugs act as agonists at the parathyroid hormone receptor, and once-daily subcutaneous administration results in stimulation of osteoblastic activity and increased bone formation and bone strength. These agents should be reserved for patients at high risk of fractures and those who have failed or cannot tolerate other osteoporosis therapies. Both drugs have been associated with hypercalcemia, orthostatic hypotension, and an increased risk of osteosarcoma in rats. Selective estrogen receptor modulators Lower estrogen levels after menopause promote proliferation and activation of osteoclasts, and bone mass can decline rapidly. However, since estrogen may increase the risk of endometrial cancer (when used without a progestin in women with an intact uterus), breast cancer, stroke, venous thromboembolism, and coronary events, it is no longer recommended as a preventive therapy for osteoporosis. It has estrogen-like effects on bone and estrogen antagonist effects on breast and endometrial tissue. Therefore, raloxifene increases bone density without increasing the risk of endometrial cancer, and it decreases the risk of invasive breast cancer. Because it has not been shown to reduce nonvertebral or hip fractures, raloxifene should be used as an alternative to bisphosphonates or denosumab in the treatment of postmenopausal osteoporosis. Adverse effects include hot flashes, leg cramps, and increased risk of venous thromboembolism. The drug reduces bone resorption, but it is less effective than other agents, and is no longer routinely recommended for the treatment of osteoporosis. A unique property of calcitonin is relief of pain associated with osteoporotic fracture. Therefore, calcitonin is sometimes prescribed for the short-term treatment of patients with a recent painful vertebral fracture. The intranasal formulation is most commonly used in osteoporosis, and adverse effects include rhinitis and other nasal symptoms. Food and other medications decrease absorption of bisphosphonates, which are already poorly absorbed (less than 1%) after oral administration. Denosumab is administered every 6 months, and risedronate is administered daily, weekly, or monthly. Teriparatide is a parathyroid hormone analog that has anabolic effects on bone through stimulation of osteoblast activity. The other medications work primarily by inhibiting osteoclast activity (inhibition of bone resorption). Her daily medications include methotrexate, prednisone, metformin, hydrochlorothiazide, and lisinopril, and calcium carbonate as needed for heartburn symptoms. Which of her medications is most likely to contribute to the risk of developing osteoporosis? Glucocorticoids (for example, prednisone at a dose of ≥ 5 mg per day for greater than 3 months) are a significant risk factor for osteoporosis. The other medications have not been shown to increase the risk of osteoporosis, and calcium carbonate and hydrochlorothiazide (diuretic that increases calcium retention) may be beneficial for patients at risk of osteoporosis. Bisphosphonates are first-line therapy for osteoporosis in postmenopausal women without contraindications. Raloxifene is an alternative that may be less efficacious (especially for nonvertebral and hip fractures), and calcitonin is not recommended. Which is the primary reason oral bisphosphonates should be used with caution in this patient? Bisphosphonates are known to cause esophageal irritation and should be used with caution in a patient with a history of erosive esophagitis. Liver disease is not a contraindication to bisphosphonate use, since bisphosphonates are mainly cleared via the kidney. Thyroid disease is not a contraindication to bisphosphonate use, although overaggressive replacement of thyroid may contribute to osteoporosis. Patients need to remain upright for 60 minutes after ibandronate (30 minutes for other bisphosphonates). Bisphosphonates, unlike raloxifene, are not associated with blood clots and leg cramps. Use of the recombinant parathyroid hormone teriparatide should be limited to 2 years. Risk of which adverse effect might warrant consideration of a drug holiday from alendronate in this patient? Atypical femur fractures are associated with long-term use of bisphosphonates (greater than 5 years). Therefore, a drug holiday might be considered since the patient has had no fractures. Esophagitis, while a side effect of bisphosphonate therapy, can be prevented with appropriate administration. Osteosarcoma is associated with the parathyroid hormone analogs, and rhinitis is associated with intranasal calcitonin. Overview Antimicrobial therapy takes advantage of the biochemical differences that exist between microorganisms and human beings. Antimicrobial drugs are effective in the treatment of infections because of their selective toxicity; that is, they have the ability to injure or kill an invading microorganism without harming the cells of the host. In most instances, the selective toxicity is relative rather than absolute, requiring that the concentration of the drug be carefully controlled to attack the microorganism, while still being tolerated by the host.
Escitalopram 10mg visa. Eddie Brock Bonds to Venom & Fights God Carnage Explained (Part 1 of 3).
Abnormalities detected by stress testing require coronary angiography to investigate the need for coronary stenting or even coronary artery bypass cheap 20mg escitalopram mastercard papa roach anxiety. It may also be reasonable to perform coronary angiography on high-risk patients with significant comorbidities or a pronounced history of cardiac problems with unremarkable stress testing purchase 20 mg escitalopram with visa anxiety symptoms menopause. Recurrent urinary tract infections or bladder dysfunction requires urodynamic testing and urology consultation purchase escitalopram 10 mg anxiety shortness of breath. Abnormal results require hematology consultation and a plan for therapeutic measures in the perioperative period buy cheap escitalopram 10mg on line anxiety neurosis. In addition to electrolyte screening, a complete history and physical examination, electrocardiogram, chest X-ray, and laboratory examination should be performed just prior to the operation to uncover any possible health derangements since the last physician visit. Intraoperative Care the degree of invasive monitoring during the operation should reflect the extent of the recipient’s comorbidities. Central venous catheters are commonly introduced to guide intraoperative and postoperative fluid management. Continuous arterial blood pressure monitoring is also quite common and facilitates blood pressure management during the case. It is justified when recipients have significant cardiac dysfunction, valvular abnormalities, or significant pulmonary artery hypertension. A 20-F three-way Foley catheter is useful to inflate the bladder with saline that greatly facilitates the ureteroneocystostomy. After completion of this anastomosis, urine output is checked frequently to guide fluid resuscitation. Optimizing the chance of immediate graft function requires careful communication and coordination between anesthesia and surgical teams. Most patients, however, can receive appropriate care on a solid-organ transplant ward provided there is mechanism for proper fluid resuscitation. This can be challenging, with the voluminous urine output often encountered with immediate graft function. The basis of the resuscitation is the equivalent replacement of urine output milliliter for milliliter, which is measured hourly. After 24 hours, the fluid replacements are converted to a continuous rate between 100 and 150 mL per hour based on the recipient weight and kidney function. Serial blood counts, coagulation profiles, and chemistries should be obtained in the postoperative period. Electrolyte abnormalities, especially hyperkalemia, hypokalemia, hypomagnesaemia, and hypocalcaemia are common and should be corrected. Serial troponins should be obtained to exclude myocardial ischemia with select recipients with significant cardiac comorbidity. Kidney transplant recipients are prone to complications owing to their significant comorbidities, intense immunosuppression, and variable graft function. It is estimated that between 15% and 30% of high-risk transplant candidates will require specific critical care. Diuresis on its own may be a result of the urine produced by the recipient’s native kidneys or the residual effect of diuretics infused during the operation. Intensivists must be aware that ultrasound can rule out surgical complications that require immediate therapeutic maneuvers to salvage the graft including clearing of arterial or venous thromboses. Most importantly, surgical complications need to be ruled out, most notably, thrombosis with a Doppler ultrasound. Acute Rejection Acute rejection in kidney transplantation is of great significance, but a comprehensive review is beyond the scope of this chapter. There are two types of acute rejection, cellular rejection and antibody-mediated rejection; both can diminish graft function and survival [16]. At present, this diagnosis is secured with a kidney biopsy, although there are efforts underway for noninvasive diagnostics. After vascular thrombosis and urologic complications are ruled out, the next step is often a biopsy to rule out rejection. Acute cellular rejection, which is a lymphocytic attack against donor tissue, is most often treated with a course of steroids or thymoglobulin. In antibody-mediated rejection, preformed or de novo alloantibodies target capillary endothelium and by activating the complement system can result in rapid destruction of the allograft. It may be recurrent or de novo, with the patient’s calcineurin inhibitor being a well-known causative agent [17]. Surgical Complications Leading to Early Graft Dysfunction Hemorrhage after surgery is always a possibility but is rare in kidney transplantation because the surgical field is confined to the retroperitoneal space, so bleeding usually tamponades. Bleeding is suspected if the patient is tachycardic, hypotensive, oliguric, and requiring blood transfusions. Subscapular bleeding in the allograft is an entirely different matter, as it can lead to compression and quick deterioration of allograft function. If this is recognized on Doppler ultrasound with evidence of compression, immediate reexploration is imperative to release the hematoma. Arterial thrombosis is a devastating complication in kidney transplantation, as the renal arteries are end arteries without collateralization. Therefore, arterial thrombosis almost invariably results in graft loss; however, fortunately it is rare (0. As mentioned earlier in the chapter, impaired graft function or a sudden change in urine output should elicit a Doppler ultrasound, which is usually diagnostic when thrombosis is present. If discovered early, within hours, graft salvage is possible although most cases result in irreparable damage necessitating transplant nephrectomy. Unidentified intimal flaps, allograft damage in the procurement, donor–recipient size discrepancy, hypotension, and technical difficulty with multiple arteries in the donor or diseased iliac vessels in the recipient are all identified causative factors [18]. It is most often diagnosed within a few days after the transplant and is characterized by sudden onset of pain and graft swelling, hematuria, and, in the case of iliofemoral thrombosis, an edematous leg. In addition to the vein thrombosis, the Doppler ultrasound often shows reversal of the diastolic flow in the arterial system and an enlarged kidney possibly surrounded by hematoma. Urgent allograft nephrectomy is necessary in complete thrombosis to prevent kidney rupture and devastating hemorrhage. It is most often caused by kinking of the anastomosis, intimal injury during organ procurement, pressure on the vein secondary to a fluid collection (i. Recipients with renal artery stenosis require percutaneous balloon dilation, or if unsuccessful, surgical repair. Urologic complications are much more common than vascular complications, but if addressed systematically, rarely threaten the viability of the allograft. Urologic complications, including hematuria, urine leaks, and ureteral stenosis, range from 5% to 14% [20]. Hematuria is not uncommon from operating on the distal ureter and bladder and often resolves within 24 hours; however, clot formation leading to obstructive uropathy can occur, especially with poor initial urine flow. Occasionally, hematuria can be caused by posttransplant biopsies with blot clots forming in the renal pelvis. The presentation can be quite varied, including wound drainage, persistent tenderness, fevers, or general swelling. They are also commonly diagnosed on surveillance Doppler ultrasound where a large perinephric fluid collection is aspirated and found to have a high creatinine content. More significant leaks are approached with immediate exploration and reimplantation of the ureter or with percutaneous maneuvers to maximize drainage for 4 to 8 weeks.
This system is based on standard parameters periodically obtained by bedside nurses (see Table 2 buy 10 mg escitalopram free shipping anxiety symptoms jaw clenching. Abdominal examination may reveal hypoactive or hyperactive bowel sounds order escitalopram 5mg on-line anxiety symptoms gad, abdominal distension order escitalopram 5 mg on line anxiety symptoms lingering, diffuse or discrete areas of tenderness order 20 mg escitalopram otc anxiety quotes tumblr, and guarding or rebound in the patient whose primary focus of infection lies in the gastrointestinal tract (Chapter 8). Costovertebral angle tenderness combined with a history of dysuria raises the possibility of pyelonephritis as the primary focus of infection (Chapter 9). The skin should be carefully examined, particularly in areas where intravascular devices have been inserted. Any evidence of purulence, tenderness, or significant erythema should encourage immediate removal of the intravascular device. In cases of meningococcemia, petechial skin lesions are commonly found, and if not quickly treated with systemic antibiotics, these lesions can rapidly progress to larger areas of skin ecchymosis that reflect similar events taking place in other organs. The temperature of the extremities and the skin overlying the platella should be assessed. Early septic shock is associated with warm extremities; however, as the disease progresses vasoconstriction will eventually lead to cool and “clammy” extremities and mottling of the skin overlying the platella. Other indications of hypoperfusion include delayed capillary refill, oliguria, and altered mentation. Test for occult blood in the stool and gastrointestinal secretions should be performed. History the history should focus on symptoms that may point to the primary infection that has precipitated sepsis. Patients with pulmonary and intra- abdominal infections have the highest incidence of severe sepsis with positive blood culture. Therefore, caregivers need to ask the patient and family members questions designed to explore these two possible diagnoses. For pulmonary infection, caregivers should inquire about cough, sputum production, color of sputum, shortness of breath, pleuritic chest pain, and confusion (see Chapter 4). And for intra-abdominal infections, questions should be focus on abdominal pain, constipation, diarrhea, nausea, and vomiting as well as past history of abdominal surgery and/or bowel problems (see Chapter 8). History and examination should focus on identifying the primary focus of infection. Every hour of delay in initiating appropriate treatment increases the mortality of sepsis by 7. To assure an appropriately rapid and effective response, guidelines recommend initiating the sepsis six bundle whenever sepsis is being considered. Deliver high flow oxygen—Oxygen delivery to all organ systems is critical for survival. Draw blood cultures—Assure blood culture volume is 20 cc per sample to maximize sensitivity. With the exception of endocarditis spacing, blood cultures over time have not proven to be helpful, and this approach can delay the initiation of antibiotics. There is no need to exceed four blood cultures because there is no improvement in sensitivity by drawing additional cultures unless there is dramatic change in the patient’s fever pattern. Excess number of blood cultures lowers hemoglobin levels and has the potential to reduce oxygen delivery to the organs. Delays in initiating appropriate antibiotics greatly decrease the patient’s likelihood of survival. If appropriate antibiotic therapy is withheld for 36 hours, the mortality is nearly 100%. However, logistical problems with blood culture sampling should never be allowed to delay antibiotic administration beyond the first hour. Activate the Sepsis 6 bundle and complete within 1 hour; avoid transfer until complete: a) Deliver high flow oxygen. Empiric antibiotic therapy must take into account a) the presumed primary anatomic site of the infection. A serum lactate level of ≥4 mM/L suggests the patient is progressing from severe sepsis to septic shock. Antibiotic Therapy the initial empiric antibiotic regimen should be chosen based on the suspected primary site of infection (see Table 2. Coverage is then chosen to assure treatment of the most common pathogens known to infect that specific site. Sepsis associated with certain organisms, including Pseudomonas aeruginosa and Candida species, may result in higher mortality rates. When the clinical conditions raise the probability of these organisms, the empiric regimen should include coverage for these pathogens. The susceptibility of the pathogens within each institution and local unit must also be considered when designing an empiric therapy. When gram- negative bacteria grown from the bloodstream are resistant to the empiric regimen, the risk of death is significantly higher. Therefore, the empiric regimen should always take into account the local antibiotic susceptibility patterns. Furthermore, if a patient has been hospitalized for significant period and develops nosocomial sepsis, coverage should include previously isolated pathogens from the suspicious site. In 24-48 hours after blood culture results are available, the antibiotic regimen must be adjusted, with narrower spectrum antibiotics utilized whenever possible to reduce the likelihood of selecting for highly resistant pathogens. Therefore, clinicians need to closely monitor mean blood pressure, serum lactate, as well as skin color and temperature of the extremities. When serum lactate levels rise to >4 mM/L, mortality increases to nearly 40% as compared to <15% for patients with serum lactate levels of <2 mM/L. Given the far greater expense of colloids, crystalloids are considered by most experts to be the treatment of choice. In the past, dopamine was recommended as the vasopressor of choice; however, a recent meta- analysis has revealed that when compared to norepinephrine, dopamine increases mortality by 1. This agent acts on both alpha-1 and beta-1 adrenergic receptors producing potent vasoconstriction as well as a modest increase in cardiac output. In the past, lowdose dopamine was recommended to maintain renal output; however, given the increased risk of arrhythmias, this approach has recently been abandoned by most experts. The patient is periodically scored based on vital sign parameters, metabolic studies, and underlying disease. This score closely correlates with the severity and progression of disease as well as mortality; scores theoretically can range from 0 to 63, the higher the score the worse the prognosis. Vasoconstrictor of choice is norepinephrine (Levophed), and dopamine increases the risk of arrhythmias. Manifestations of thrombosis can include cyanosis or gangrene of fingers or toes and hemorrhagic necrosis of the skin (most prominent with meningococcemia). Bleeding will first be seen at sites of surgical intervention and at intravascular device placement sites.