University of Scranton. C. Pyran, MD: "Buy Nebivolol online in USA - Proven online Nebivolol OTC".
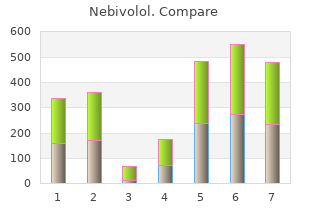
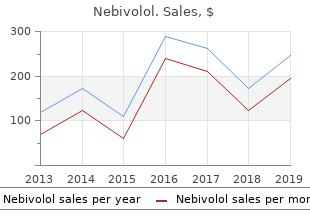
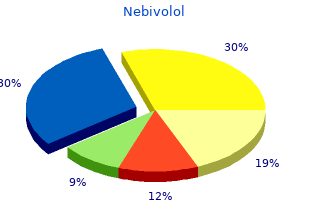
This is the time needed for the drug’s plasma concentration to decrease by 50% from a steady-state concentration cheap nebivolol 5mg with mastercard pulse pressure variation ppt. For example cheap 5mg nebivolol overnight delivery arteria volaris indicis radialis, the active metabolite of morphine discount nebivolol 2.5 mg with amex heart attack song, morphine-6-glucuronide cheap nebivolol 5mg online hypertension signs and symptoms, can accumulate in patients with renal impairment. It is also important to take into account the delay between the administration of an opioid and its effect, which is defined as the blood–effect site equilibration half-life, or t½k. This wille0 allow proper and timely dosing particularly when anticipating a stressful event (laryngoscopy, intubation, skin incision, etc. Since the t½k of morphine is about 90 minutes, it ise0 important to give an initial bolus dose or morphine at least 60 minutes before the end of surgery when using the drug for postoperative pain relief. Using known pharmacokinetic and pharmacodynamic data it can be determined what doses and plasma concentrations will permit the shortest time to awakening. For example, termination of drug infusions at plasma concentrations of propofol 1. In chronic pain patients risk factors included renal failure, sensory deafferentation, and drug–drug interactions. The required dose of naloxone depends on the pharmacokinetic and pharmacodynamic properties and the dose of the opioid that needs 1301 reversal. Postoperatively, when there is persistent apnea, opioid concentrations are often just above the threshold for respiratory depression. Intravenous administration of naloxone using incremental doses of 40 to 80 μg, to a cumulative dose of less than 400 μg, may be sufficient for breathing to resume. These drugs include blockers of potassium-channels expressed on oxygen-sensing cells of the carotid bodies and drugs that increase respiratory drive through action at α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid receptors in brainstem respiratory centers involved in rhythmogenesis. The cardiovascular side effects of opioids include bradycardia and hypotension but are generally mild at usual clinical doses. However, when combined with anesthetics, even at usual clinical doses, or in severely ill patients, opioids may produce hemodynamic instability, which requires treatment. Introduction Opioids are the most potent painkillers available in modern medicine. Traditionally opioids are used in perioperative care by anesthesiologists and other anesthesia care providers to attenuate autonomic responses to noxious (surgical) stimulation and treat acute postoperative pain. In recent years, however, there has been an exponential increase in the prescription of opioid analgesics by pain specialists and other health-care providers, such as primary care doctors, for treatment of chronic (cancer and noncancer) pain. Consequently, a significant number of patients in developed countries are exposed to these potent drugs that not only produce pain relief but also cause a variety of side effects that range from dizziness, orthostatic hypotension, nausea, and constipation to harmful and potentially lethal effects such as addiction and critical respiratory depression. The “epidemic” of opioid use by nonsurgical patients, coupled with an emphasis on aggressive and effective postoperative pain management for patients undergoing surgery, has resulted in increasingly complex postoperative pain management problems for surgical patients, and an increase in opioid-related complications for patients1 with pain in general. Many old civilizations, including the Sumerians, Egyptians, Greeks, Romans, and Chinese, used opium for nutritional, medicinal, euphoric, spiritual, and religious purposes. Just over 200 years ago, the German pharmacist and chemist Friedrich Sertürner isolated a stable alkaloid crystal from the opium sap and named it morphine after the Greek god of dreams, Morpheus. After the invention of the hypodermic syringe in 1853, the Englishman Alexander Wood was the first to inject morphine in a controlled fashion into a patient producing more than a day’s sleep. The first reported casualty from6 morphine occurred shortly thereafter when Wood injected his wife with morphine resulting in a fatal overdose from respiratory depression. Morphine revolutionized the treatment of the wounded in battlefield medicine, but euphoric and addictive properties led to the addiction of thousands of soldiers to morphine during the American Civil War. After the structure of morphine was determined in the 1920s, the synthesis of new morphine-like opioid compounds was based on chemical principles rather than empirical discoveries. In 1937, meperidine (or pethidine) became the first synthetic opioid synthesized on the basis of the central structure of morphine. Since then many synthetic and semisynthetic opioids have been produced, including the clinically important opioid antagonists naloxone and naltrexone, by replacing the N-methyl substituent in morphine with allyl and cyclopropylmethyl groups, respectively (Fig. The continued development of opioids with complex9 simultaneous actions at multiple target sites is driven by concerns that the side effect profile of potent opioids, which presents a serious risk to patients, needs to be minimized. The Endogenous Opioid System 1304 A major breakthrough in the understanding of opioid pharmacology came from a series of discoveries of opioid receptors, endogenous opioid peptides, their encoding genes, and endogenous opioid alkaloids. In rodents, various subtypes of opioid receptors have also been identified, with different pharmacologic functions. Interactions between opioid ligands and selective17 receptors have a number of important clinical effects. It is also a norepinephrine reuptake inhibitor in the spinal cord, activating α -adrenergic receptors in the spinal cord dorsal2 horn. However, due to synergy between the two mechanisms of action, tapentadol produces potent analgesia and is useful in the treatment of moderate-to-severe acute and chronic pain. Tapentadol differs from tramadol due to its lack of serotonergic activity resulting in a lower incidence of nausea and vomiting. Tapentadol produces analgesic effects in chronic neuropathic pain patients by (re)activation of descending inhibitory pathways. In various animal models of acute and chronic (neuropathic) pain,9 cebranopadol produces potent antinociception with a favorable side effect profile. Opioid Mechanisms 1306 Central Opioid Analgesia Whereas nociception is the neural process of encoding and processing of noxious stimuli that can potentially (or actually) damage tissue, pain is the26 subjective translation of these stimuli into a perception or sensation. Opioids modify both nociception and the perception of a noxious stimulus (emotional coloring of pain). Different types of peripheral sensory nociceptors, often free nerve endings, are stimulated by tissue damage. The resulting pain information is transmitted to the spinal cord by two types of small diameter peripheral afferent fibers: slow conducting, unmyelinated C-fibers (which cause a dull burning pain) and faster, thinly myelinated Aδ fibers (which cause sharp, pricking pain). Projection neurons from these laminae give rise to the ascending pathways of the spinothalamic tract. Opioid receptors are further abundantly29 present in the spinal cord dorsal horn at pre- and postsynaptic locations. In the superficial laminae of the dorsal horn, local neuronal circuits process both ascending and descending pain pathways and are regulated by local endogenous opioid circuits. The electrically stimulated30 sites overlap with the opioid receptor sites and with opioid-containing interneurons, linking together the actions of exogenously applied analgesic stimuli and endogenous opioid systems. The endogenous opioid system is activated under stressful conditions, as demonstrated by the delayed onset of pain by soldiers wounded in battle. The endogenous opioid system also mediates placebo-induced analgesia, a reduction of pain resulting from an expectation of pain relief. Since naloxone blocks this effect it is assumed that39 endogenous opioids are released during the nose twitch. In humans, tapentadol is an example of an opioid that induces analgesia through activation of descending pathways (Fig. Descending inhibition is activated in various higher brain centers, including the rostral ventromedial medulla, periaqueductal gray, amygdala, cingulate cortex, insula, and orbitofrontal cortex.
For each combination of gas-driving pressure buy nebivolol 5mg lowest price blood pressure chart download excel, jet orifice discount 2.5mg nebivolol fast delivery heart attack heart attack, and bronchoscope diameter cheap 5mg nebivolol otc blood pressure examples, only one inflation pressure can be attained buy generic nebivolol 5 mg online blood pressure 9862, regardless of the volume or compliance of the lung. As long as the proximal end of the bronchoscope is open, the system is strictly pressure limited, and the pressure does not increase because of obstruction at the distal end. Pressure varies inversely with the cross-sectional area of the bronchoscope, so insertion of a suction catheter or biopsy forceps into the lumen causes the intratracheal pressure to increase. Provided there is not a tight fit between the bronchoscope and the airway, the risk of barotrauma is low. The advantages of the Sanders system are that because continuous ventilation is possible (because the presence of an eyepiece is not necessary for ventilation of the lungs), the duration of the bronchoscopy procedure is 2620 minimized, but the efficiency also permits extended bronchoscopy. Ventilation of the lungs may be achieved by connecting a mechanical ventilator to an anesthesia circuit that is connected to the bronchoscope side arm. One disadvantage of this ventilation technique is the presence of a leak of anesthesia gases, and consequentially, light anesthesia. Fiberoptic Bronchoscopy New generations of fiberscopes, with their improved optics and smaller diameters, have revolutionized bronchoscopy. Nasal fiberoptic bronchoscopy under topical anesthesia is well tolerated by most awake patients. The administration of an antisialagogue such as glycopyrrolate is useful in reducing secretions. Oral insertion is also possible in both awake and asleep patients and should be performed with a bite block in place to prevent damage to the bronchoscope. In all patients, insertion of the fiberoptic bronchoscope is associated with hypoxemia. The average decline in PaO2 is 20 mmHg and lasts for 1 to 4 hours after the procedure. This can be provided using mouth- held nasal prongs, a special face mask with a diaphragm through which the fiberscope can be passed, or an endotracheal tube with a T-piece diaphragm adapter. During and after fiberoptic bronchoscopy, patients experience increased 2621 airway obstruction. These changes are believed to be secondary to direct mechanical activation of irritative reflexes in the airway and, possibly, to mucosal edema. They may be avoided if atropine, either intramuscular or aerosolized into the airway, is administered before the procedure. If suction at 1 atm is applied to the fiberscope, air is removed at a rate of 14 L/min. The adult fiberscope can be passed through endotracheal tubes of 7 mm or greater internal diameter. Clearly, passage through an endotracheal tube decreases the cross-sectional area available for ventilating the patient, so if fibroscopy is planned, an endotracheal tube of the largest possible diameter should be used. A postendoscopy chest radiograph is advisable to exclude the presence of mediastinal emphysema or pneumothorax. In patients whose tracheas are intubated with endotracheal tubes of less than 7 mm internal diameter, use of pediatric fiberscopes, which have smaller diameters, would be more appropriate. The suction channel of the adult fiberoptic bronchoscope has been used to oxygenate and ventilate the lungs of patients. By attaching a jet ventilation system (similar to that used to drive the Sanders injector for rigid bronchoscopy) to the suction connection at the head of a fiberoptic bronchoscope, successful ventilation of the lungs of patients undergoing gynecologic procedures was achieved. This technique permitted adequate ventilation of patients with normally compliant lungs and chest walls. Ventilation of the lungs should be performed only with the tip of the instrument in the trachea because a more peripheral location may produce barotrauma. The lasers may be introduced into the bronchial tree through a fiberoptic bundle passed via the suction port of the fiberoptic bronchoscope. Complications of Bronchoscopy Complications of rigid bronchoscopy include mechanical trauma to the teeth, hemorrhage, bronchospasm, loss of a sponge, bronchial or tracheal perforation, subglottic edema, and barotrauma. Nevertheless, complications may arise owing to overdose with topical anesthetic, insertion trauma, local trauma, hemorrhage, upper airway obstruction related to passage of the instrument through an area of tracheal stenosis, hypoxemia, and bronchospasm. In most cases, it is best to intubate the trachea with an endotracheal tube after bronchoscopy under general anesthesia. This permits avoidance or treatment of some of these problems, particularly the increased airway irritability. Intubation also facilitates effective suctioning of the trachea and bronchi, and allows the patient to recover more gradually from general anesthesia. Diagnostic Procedures for Mediastinal Mass Patients with an anterior mediastinal mass may present a special problem for the anesthesiologist. Although such masses may cause obvious superior vena cava obstruction, they may also cause obstruction of major airways and cardiac compression, which are less obvious and may become apparent only on induction of anesthesia. Many cases of anesthetic-related airway compression from anterior mediastinal mass have been reported. In one case, total occlusion of the trachea starting 2 to 3 cm above the carina and extending to both main stem bronchi was observed, and a bronchoscope was passed through the obstruction. These findings suggested potential obstruction with onset of anesthesia; radiation therapy to the mediastinum was commenced, after which the flow–volume studies showed improved function. In a subsequent series of 105 patients with mediastinal masses, the incidence of intraoperative cardiorespiratory complications was 38%, and the incidence of 2623 postoperative respiratory complications was 11%. In another series of patients with mediastinal mass, four patients had abnormal spirometry but underwent general anesthesia without sequelae. However, a serious potential disadvantage of preoperative radiation therapy is that it may affect tissue histologic appearance, thereby preventing an accurate diagnosis. Furthermore, if the patient is a child, it may be difficult to obtain tissue samples under local anesthesia. No fatalities occurred in a series of 44 patients aged 18 years of age or younger with anterior mediastinal masses who underwent general anesthesia before radiation or chemotherapy. Preoperative evaluation of a patient with an anterior mediastinal mass to avoid life-threatening total airway obstruction is shown in Figure 38-21. If such obstruction occurs, it may be relieved by passage of a rigid bronchoscope or anode tube past the obstruction, by direct laryngoscopy,168 or by changing the position of the patient. Airway collapse and inability to ventilate has been reported in a previously asymptomatic patient with a mediastinal mass despite spontaneous ventilation with an inhaled anesthetic and an endotracheal tube. Positive-pressure ventilation was impossible, a rigid bronchoscopy was requested and the surgeons began to prepare femoral vessel access for emergent cardiopulmonary bypass. Fortunately, the airway patency was re-established when the patient’s spontaneous respiratory efforts improved as he awoke from general anesthesia. The authors emphasize the need for immediate availability of a rigid bronchoscope and that if a patient is at high risk, then serious 2624 consideration should be given to insertion of the femoral cannulas with cardiopulmonary bypass standing by before general anesthesia is induced.
Although a single isolated fourteenth-generation bronchiolar airway may have greater resistance to air flow compared to a bronchus cheap nebivolol 2.5 mg overnight delivery pulse pressure guide, the overall total resistance in a system is also dependent on the number of parallel pathways present purchase 2.5 mg nebivolol amex heart attack and vine. The overall total resistance of the system will be less than any individual tube’s resistance 5 mg nebivolol sale blood pressure questions and answers, as illustrated by the equation: The anatomy of the tracheobronchial tree is organized in such a way that there is an increase in total parallel pathways and total cross-sectional area with each generation toward the periphery buy discount nebivolol 5mg on-line blood pressure of 90 60. Therefore, total airway resistance to gas flow is lower at the periphery compared to the large bronchi. The exponential increase in total cross-sectional area of parallel airways 964 toward the lung periphery also affects airflow velocity. Similar to airflow resistance, velocity is inversely proportional to a system’s overall total cross- sectional area. Therefore, airflow velocity at the lower generations of the tracheobronchial tree is lower than that of the bronchi. In other words, the velocity of airflow decreases from the trachea down to the peripheral distal airways. During normal quiet ventilation, gas flow within convective airways is mainly laminar. Gas Diffusion Diffusion within a gas-filled space is random molecular motion that results in complete mixing of all gases. In the distal airways of the lung beginning with the terminal bronchioles (sixteenth airway generation), diffusion becomes the predominant mode of gas transport. Once gas reaches the small alveolar ducts, alveolar sacs, and alveoli, both diffusion and regional V˙/Q˙ relationships influence gas transport. Historically, clinicians assumed defects in gas diffusion were responsible for arterial hypoxemia. However, the most frequent cause of arterial hypoxemia is shunt effect (see Ventilation–Perfusion Relationships section). In this sense, carbon dioxide is 20 times more diffusible across human membranes than is oxygen; therefore, carbon dioxide crosses alveoli easily. As a result, hypercapnia is never the result of defective diffusion; rather, it is the result of inadequate alveolar ventilation relative to carbon dioxide production. The most common reason for a measured decrease in diffusing capacity (see Pulmonary Function Testing section) is mismatched ventilation and perfusion, which functionally results in a decreased surface area available for diffusion. Distribution of Ventilation and Perfusion The efficiency with which oxygen and carbon dioxide exchange at the alveolar–capillary level highly depends on the matching of capillary perfusion and alveolar ventilation. At this level, the marriage between the lung and the circulatory system must be well matched and intimate. Distribution of Blood Flow Blood flow within the lung is mainly gravity dependent. Because the alveolar– capillary beds are not composed of rigid vessels, the pressure of the 965 surrounding tissues can influence the resistance to flow through the individual capillaries. Thus, blood flow depends on the relationship between pulmonary artery pressure (P ), alveolar pressure (P ), and pulmonary venous pressurepa A (P ) (pv Fig. Pulmonary artery pressure always exceeds pulmonary venous pressure, which is subatmospheric in Zone 1. InA pa pv Zone 1, alveolar pressure transmitted to the pulmonary capillaries promotes their collapse, with a consequent theoretical blood flow of zero to this lung region. However, in conditions of decreased pulmonary artery pressure, such as hypovolemic shock, Zone 1 enlarges, thus increasing alveolar dead space ventilation. Zone 2 occurs from the lower limit of Zone 1 to the upper limit of Zone 3, where P > P > P. The pressure difference between pulmonary arterypa A pv and alveolar pressure determines blood flow in Zone 2. Well-matched ventilation and perfusion occur in Zone 2, which contains the majority of alveoli. Finally, Zone 3 occurs in the most gravity-dependent areas of the lung where P > P > P and blood flow is primarily governed by thepa pv A pulmonary arterial to venous pressure difference. Because gravity also increases pulmonary venous pressure, the pulmonary capillaries become distended. Thus, perfusion in Zone 3 is lush, resulting in capillary perfusion in excess of ventilation, or physiologic shunt. Distribution of Ventilation Alveolar pressure is the same throughout the lung; therefore, the more negative intrapleural pressure at the apex (or the least gravity-dependent area) results in larger, more distended apical alveoli than in other areas of the lung. The transpulmonary pressure (Paw − P ), or distending pressure of thepl lung, is greater at the top and lower at the bottom, where intrapleural pressure is less negative. Despite the smaller alveolar size, more ventilation is delivered to dependent pulmonary areas. The decrease in intrapleural pressure at the base of the lungs during inspiration is greater than at the apex because of diaphragmatic proximity. Thus, because the dependent area of the lung generates the greatest change in transpulmonary pressure, more gas is sucked into dependent areas of the lung. During a spontaneous breath, the largest portion of the tidal volume also reaches the gravity-dependent part of the lung. Thus, the nondependent area of the lung receives a lower proportion of both ventilation (V ) and perfusion (Q), and dependent lung receives greaterA proportions of ventilation and perfusion. Nevertheless, ventilation and perfusion are not matched perfectly, and various V˙/Q˙ ratios result throughout the lung. The ideal V˙/Q˙ ratio of 1 is believed to occur at approximately the level of the third rib. Above this level, ventilation occurs slightly in excess of perfusion, whereas below the third rib the V˙/Q˙ ratio becomes less than 1 (Fig. In a simplified model, gas exchange units can be divided into normal (V˙/Q˙ 1:1), dead space (V˙/Q˙ = 1:0), shunt (V˙/Q˙ = 0:1), or a silent unit (V˙/Q˙ = 0:0) (Fig. Although this model is helpful in understanding V˙/Q˙ relationships and their influences on gas exchange, V˙/Q˙ really occurs as a continuum. In the lungs of a healthy, upright, spontaneously breathing individual, the majority of alveolar–capillary units are normal gas exchange units. The V˙/Q˙ ratio varies between absolute shunt (in which V˙/Q˙ = 0) to absolute dead space (in which V˙/Q˙ = ∞). Rather than absolute shunt, most units with low V˙/Q˙ mismatch receive a small amount of ventilation relative to blood flow. Similarly, most dead space units are not absolute, but rather are characterized by low blood flow relative to ventilation. During acute lung injury and adult respiratory distress syndrome, areas of low V˙/Q˙ matching commonly lie adjacent to areas of high V˙/Q˙ matching. Thus, the West lung50 zone model should be used to aid the understanding of pulmonary physiology and not be regarded as an incontrovertible anatomic truism. In Zone 2, arterial pressure exceeds alveolar pressure, but alveolar pressure exceeds pulmonary venous pressure (Ppv). Flow in Zone 2 is determined by 967 the arterial–alveolar pressure difference (Ppa − P ), which steadily increases down theA zone. In Zone 3, pulmonary venous pressure exceeds alveolar pressure, and flow is determined by the arterial–venous pressure difference (Ppa − Ppv), which is constant down this pulmonary zone. However, the pressure across the vessel walls increases down the zone so their caliber increases, as does flow.
Electrocardiographic abnormalities and serum magnesium in patients with subarachnoid hemorrhage cheap 5mg nebivolol overnight delivery arrhythmia heart rate monitor. Correction of ionized plasma magnesium during cardiopulmonary bypass reduces the risk of postoperative cardiac arrhythmia nebivolol 2.5mg discount blood pressure gradient. It occurs in approximately 1% to 5% of patients receiving heparin and is associated with morbidity from thromboembolic complications nebivolol 5 mg otc arteria3d full resource pack. Introduction Recent focus on quality buy nebivolol 5mg otc arteria coronaria derecha, safety, and cost effectiveness in health care extends into the practice of transfusion medicine. Patient-centered blood management emphasizes the use of evidence-based decisions and blood conservation strategies. Therefore, it is imperative for the anesthesia provider to understand the treatment benefits, the rare and common adverse effects, and the specific therapeutic details of blood product preparation, conservation, and delivery in order to best manage their patients. This chapter begins with a review of primary and secondary hemostasis, fibrinolysis, and regulation of the coagulation pathway. We continue with a 1087 description of the most common coagulation profile tests, followed by the method for blood product collection and storage. The therapeutic indications and risks associated with blood component therapy are discussed at length. The chapter also includes extensive clinical sections discussing congenital and acquired deficiencies in hemostasis and coagulation, as well as an up-to-date presentation of available pharmacologic treatment medications to maintain a balanced hemostatic mechanism. Hemostasis and Coagulation Primary Hemostasis Blood must not only be maintained as a fluid in normal circulation, but also be capable of forming a solid clot to stanch leaks in the vascular wall, and then dismantling the clot when the need has passed. This delicate equilibrium between anticoagulation and coagulation is maintained by a complex system of counterbalanced blood proteins and cells (platelets). Many congenital and acquired disorders can push the system toward either bleeding or thrombosis. The patient care team has a number of tests to evaluate the system, and many therapeutic modalities to correct these imbalances. Platelets adhere to sites of endothelial disruption, undergo activation to recruit more platelets and amplify the platelet response, and then cross-link with fibrin, the end product of the plasma clotting factor cascade, to form a platelet plug. Many pathway intermediaries and other elements are not shown, but are reviewed elsewhere. Activation Platelet activation can be mediated by numerous signaling pathways from the platelet surface (Fig. Calcium ions catalyze release of dense granules and α-granules at the platelet surface. They also release circulating microparticles and attract and activate leukocytes; these features further contribute to hemostasis and also play a role in inflammation. The fibrin binding can also4 enmesh the platelets, contributing to the formation of the platelet plug in the convergence of the platelet and clotting factor systems. Inhibition To maintain hemostatic balance, platelets are naturally inhibited in their endothelial environment. Secondary Hemostasis Clotting factors in the plasma are activated at sites of endothelial injury and assemble in enzymatic complexes to activate thrombin. Thrombin then amplifies production of itself by activating other more efficient enzymes, which propagate a thrombin burst. Thrombin also converts fibrinogen to fibrin, which cross-links with activated platelets to form the platelet plug. Each of the three enzymatic complexes in the clotting process consists of four parts: an enzyme in the serine protease family, a cofactor, a plasma membrane phospholipid surface such as the platelet, and calcium ion (Ca2+). The proteases convert other clotting factors from their inactive circulating configuration to an active form (termed [factor number] a). This is a high-efficiency intrinsic-pathway “tenase,” which provides many times more Xa for more prothrombinase complex. Ultimately, thrombin cleaves fibrinogen to fibrin monomers, which then polymerize extensively. Inhibition of Clotting Factors 1092 The clotting pathways have three main regulatory inhibitors (Fig. Serpins disrupt the active sites and increase the clearance of their target proteases. Protein C-ase is an enzymatic complex with the same four-part structure as the coagulation complexes above: an enzyme, thrombin, its cofactor thrombomodulin, phospholipid, and Ca2+. Protein S is thought to be a cofactor for protein C; both are vitamin K–dependent. Urokinase is secreted from the endothelium, monocytes, macrophages, and urinary epithelium. These cells also bind plasminogen with two receptors, the annexin A2 complex and the urokinase receptor, which facilitate its conversion to plasmin. Clear chevron: antifibrinolytic medications blocking the lysine-binding sites on plasminogen. These drugs are lysine analogues that block the lysine-binding sites of plasminogen, preventing it from acting on fibrin. Laboratory Evaluation of Hemostasis The first screening test for hemostatic problems should always be the patient’s medical history. The nature of any abnormal bleeding is10 helpful; dermal or mucosal bleeding may suggest platelet dysfunction, whereas hemarthroses or soft tissue bleeding suggests factor deficiencies. Besides any direct past history of bleeding, thrombosis, or laboratory abnormalities, the patient’s experience with hemostatic challenges such as surgery, dental procedures, and menstruation may help rule-out clinical 1095 problems or suggest a lifelong congenital or more recent acquired disorder. The family history is helpful in diagnosing a congenital problem and the possible pattern of inheritance. Anticoagulants and antiplatelet medications, including over-the-counter drugs, should always be reviewed before ordering laboratory analysis. Laboratory Evaluation of Primary Hemostasis The normal automated platelet count in adults is approximately 150,000 to 400,000/μL. The peripheral blood smear should be examined in specimens with abnormal platelet counts. Microscopic review may reveal clotted specimens, artifactual platelet clumping in vitro, or abnormal platelet morphology. However, this test is invasive, labor-intensive, impractical to repeat frequently, poorly reproducible, and only modestly predictive for bleeding problems. In contrast, when both pairs are abnormal, other congenital or acquired platelet dysfunctions may be present. False negatives are common and abnormal results can also be caused by thrombocytopenia, uremia, or anemia. Several other devices test for specific antiplatelet medication effects from aspirin or P2Y12 inhibitors. Platelets are tested with multiple isolated agonists to assess their patterns of physical aggregation and, in turn, the platelets’ own agonist release.
Discount nebivolol 5 mg free shipping. INTERPOL Chad's story - fake blood pressure pills.
The term itself is derived from monere cheap nebivolol 5 mg free shipping blood pressure 700, which in Latin means to warn buy nebivolol 5 mg with mastercard blood pressure lowering, remind generic nebivolol 2.5mg fast delivery hypertension and heart disease, or admonish purchase 2.5 mg nebivolol amex arteriography. This chapter discusses the methods and biomedical devices through which anesthesiologists monitor the physiologic state of the patient during anesthesia care. These explanations are, by necessity, simplified, as the actual design of a biomedical device involves significant engineering complexity. However, the explanations are intended to be sufficient to allow the anesthesiologist to understand how the device acquires its clinical data and how that process might be compromised and the data made erroneous as well as to understand how the device works and how it may fail. There is little high-grade evidence that electronic monitors, by themselves, reduce 1761 morbidity and mortality. There is also controversy regarding the need for specific monitors in certain clinical situations, particularly in which use of the monitor in question may add significant cost or where the invasiveness of the monitoring technique may place the patient at risk of iatrogenic complications. Against these costs and risks, the anesthesiologist must balance the likely benefit from a particular monitoring technique when used and interpreted correctly. Therefore, alongside the science and engineering aspects of monitoring, there is also the clinical art of choosing how a patient should best be monitored intraoperatively. For each of the monitoring techniques, relative indications, contraindications, and common technical problems are discussed. Since 1986, these standards have emphasized the evolution of technology and practice. The current standards (which became effective on July 1, 2011) emphasize the importance of regular and frequent measurements, integration of clinical judgment and experience, and the potential for extenuating circumstances that can influence the applicability or accuracy of monitoring systems. Use of an inspired oxygen analyzer with a low concentration-limit alarm during general anesthesia. Continuously ensuring the adequacy of ventilation by physical diagnostic techniques during all anesthesia care. Continual identification of expired carbon dioxide is performed unless precluded by the type of patient, procedure, or equipment. Quantitative monitoring of tidal volume and capnography is strongly encouraged in patients undergoing general anesthesia. When administering regional anesthesia or local anesthesia, ventilation sufficiency should be assessed by qualitative clinical signs. During moderate or deep sedation, ventilation shall be evaluated by continual evaluation of qualitative clinical signs as well as monitoring for the presence of exhaled carbon dioxide unless precluded by the type of patient, procedure, or equipment. Ensuring correct placement of an endotracheal tube or laryngeal mask 1762 airway requires clinical assessment and qualitative identification of carbon dioxide in the expired gas. When using a mechanical ventilator, use of a device that is able to detect a disconnection of any part of the breathing system. During general anesthesia, circulatory function is to be continually evaluated by at least one of the following: palpation of a pulse, auscultation of heart sounds, monitoring of a tracing of intra-arterial pressure, ultrasound peripheral pulse monitoring, or pulse plethysmography or oximetry. During all anesthetics, the means for continuously measuring the patient’s temperature must be available. Every patient receiving anesthesia shall have temperature monitored when clinically significant changes in body temperature are intended, anticipated, or suspected. Monitoring of Inspired Oxygen Concentration Principles of Operation Oxygen is a highly reactive chemical species, providing many chemical and physical opportunities to detect its presence. Three main types of oxygen analyzer are seen in clinical practice: paramagnetic oxygen analyzers, galvanic cell analyzers, and polarographic oxygen analyzers. Paramagnetic gases are attracted to magnetic energy because of unpaired electrons in their outer shell orbits. Differential paramagnetic oximetry has been incorporated into a variety of operating room monitors. These instruments detect the change in sample line pressure resulting from the attraction of oxygen by switched magnetic fields. Signal changes during electromagnetic switching correlate with the oxygen concentration in the sample line. These analyzers measure the current produced when oxygen diffuses across a membrane and is reduced to molecular oxygen at the anode of an electrical circuit. The electron flow (current) is proportional to3 the partial pressure of oxygen in the fuel cell. Galvanic cell analyzers require regular replacement of the galvanic sensor capsule. In the sensor, the electric potential for the reduction of oxygen results from a chemical reaction. The current change is− − 2 2 proportional to the number of oxygen molecules surrounding the electrode. Polarographic oxygen sensors are versatile and are important components of gas machine oxygen analyzers, blood gas analyzers, and transcutaneous oxygen analyzers. Anesthesia machine manufacturers place oxygen sensors on the inspired limb of the anesthesia circuit to detect and alarm in the event that hypoxic gas mixtures are delivered to the patient. Carbon dioxide may reduce the usable lifetime of a galvanic oxygen sensor, so it is preferable to place the oxygen sensor on the inspired limb. Oxygen monitors require a fast response time (2 to 10 seconds), accuracy (±2% of the actual level), and stability when exposed to humidity and inhalation agents. The removable external oxygen sensors seen commonly on anesthesia machines, such as the Dräger Narkomed and Dräger Fabius (Dräger, Inc. These devices should be calibrated against room air (21% FiO ) daily, and also after 8 hours of use. As part2 of the preoperative checkout of the anesthesia machine, the clinician must confirm that the alarm limits of the inspired oxygen analyzer are set appropriately to alert to the presence of hypoxic mixtures. Inspired oxygen alarms cannot be relied upon to detect disconnection of the circuit. The gas mixture within the breathing circuit may become hypoxic if insufficient fresh gas flow is supplied, even if the fresh gas flow itself comprises pure oxygen. There are no clinical contraindications to monitoring inspired oxygen concentration. Common Problems and Limitations Adequate inspiratory oxygen concentration does not guarantee adequate arterial oxygen concentration. The practice of pediatric anesthesia merits additional vigilance to monitoring inspired oxygen concentration. Indications for altering inspired oxygen concentrations to facilitate anesthetics in children are common; for example, using a nitrous oxide–oxygen blend to facilitate inhalation inductions of anesthesia. Increased awareness of fire hazards in the operating room environment further reinforces the need for careful monitoring of FiO2 in pediatric anesthesia. Tonsillectomy and adenoidectomy, among the most common of surgical procedures in the pediatric anesthesia population, carry an increased risk of airway fire.