American Coastline University. Q. Roy, MD: "Buy Trimethoprim no RX - Effective Trimethoprim".
Non- ionic contrast agents are higher in cost than their ionic counterparts (rarely used currently) but have a lower incidence of adverse reactions (by a fac- tor of 9 for severe reactions) buy trimethoprim 480mg low cost antibiotics for sinus infection not penicillin. Contrast-induced nephropathy is commoner if creatinine is elevated at time of administration or if the patient has a pre- existing renal impairment order trimethoprim 960mg line antibiotics for dogs and cats, e buy discount trimethoprim 960mg on line infection journal impact factor. Plastic surgery consult should be obtained if concern regarding compartment syndrome in patients who have in excess of 100mL in extremity or severe pain/discoloration or altered perfusion buy trimethoprim 960 mg without prescription antibiotic resistance and natural selection. Its safety profle is favourable in that it does not have any of the nephro- toxicity associated with the iodinated contrast media and is more commonly associated with minor reactions such as headaches. Subsequent to this fnding, the use of gadolinium is contraindicated in patients with an eGfR of under 60 and particularly if below 30. Rapid-sequence flms are taken with a fuoroscopy unit, whilst the patient swallows barium (usually in an erect position). Indications these include the assessment of dysphagia, pain, refux disease, tracheo- oesophageal fstulae (in children), and post-operative assessment where there has been gastric or oesophageal surgery. Contraindications No absolute contraindications exist, but in all barium studies, the quality of the study relies heavily on patient co-operation, and therefore immo- bile patients who are unable to weight-bear may only be suitable for limited studies. A smooth muscle relaxant may be given as part of the routine, particularly to assess the pylorus and duodenum. Carcinoma remains the commonest cause of a flling defect in an adult (irregular, shouldered with overhanging edges). Other causes include gastric lymphoma, polyps (histology difcult to predict), and bezoars. Smooth flling defects are seen in conjunction with leiomyomas, lipomas, and metastases. In a rolling hernia, the fundus herniates through the diaphragm, but the gastro-oesophageal junction remains competent and lies below the diaphragm. Ulcers are seen either as a crater or as a projection from the luminal surface (see fig. Malignant lesions may have an associated mass and have a shallow crater and an irregular contour. With the ease of availability of endoscopy, the use of barium meals in diagnosing ulceration has declined. However, early assessment of the post-operative stomach is radiologically performed to exclude complications such as anastomotic leaks. Disadvantages include poor patient tolerance (related to intubation) and a relatively high screening dose. Indications the indications are the same for both techniques and include pain, diar- rhoea, bleeding, partial obstruction, malabsorption, overgrowth syn- dromes, assessment of Crohn’s disease activity and extent, and suspected masses. When seen with fold thickening, it may be due to Crohn’s, ischaemia, or radiotherapy. Mucosal thickening may be due to infltration by lymphoma or eosinophilia, adhesions, ischaemia, or radiotherapy. Crohn’s disease causes skip lesions, ulceration, strictures of variable length, and a high incidence of terminal ileal involvement. Disadvantages include the minimally invasive nature and the radiation associated with a Ct examination. With the current scanner resolution, the sensitiv- ity for stone disease is in the range of >95% for stones exceeding 2mm in diameter. Intravenous cholangiography this is rarely performed but may be useful in patients with biliary symptoms post-cholecystectomy or with a non-functional gall bladder. It is contrain- dicated in the presence of severe hepatorenal disease, as the side efects related to the contrast media are considerable. Ct cholangiography uses a similar contrast agent but ofers the advantage of cross-sectional assess- ment of the bile ducts. Endoscopic retrograde cholangiopancreatography the biliary and pancreatic ducts are directly flled with contrast, following endoscopic cannulation and during X-ray screening. It is particularly of value in the demonstration of ampullary lesions and to delineate the level of biliary tree obstruction in patients with obstructive jaundice. Percutaneous transhepatic cholangiography the biliary tree is directly injected with contrast, following percutaneous puncture of the liver. Disadvantages • d spatial resolution for peripheral intra-hepatic ducts and for pancreatic ductal side branches (e. Arterial phase images (20–30s after injection) i the conspicuity of lesions that are hypervascular such as hepatocellular carcinoma or focal nodular hyperplasia. Portal venous phase images are acquired at 50–70s and pro- vide maximum enhancement of background hepatic parenchyma. Lesions that are relatively hypovascular on this phase stand out such as metastases. Delayed imaging (equilibrium phase) minutes after contrast adminis- tration allows lesions that demonstrate relative washout of contrast (i. Increasingly, many institutions are replacing this technique with Ct colonography (CtC; E Virtual colo- noscopy, p. Hyoscine butylbromide (a smooth muscle relaxant) may be given to mini- mize spasm and optimize mucosal relief. Bowel preparation prior to the examination (low-residue diet and aperients) is vital to ensure that there is no faecal material, which may mask mucosal abnormalities or be mistaken for small polyps. Remember the examination is uncomfortable and requires reasonably good patient co-operation and mobility. A rectal examination or sigmoidoscopy is essential to avoid abnormalities being missed. Single vs double contrast If evaluation of the colonic mucosa is not the ° aim, then a single contrast technique will sufce. Indications Change in bowel habit, iron defciency anaemia, abdominal pain, palpable mass of suspected colonic origin, and weight loss of unknown cause. Contraindications Suspected perforation, recent rectal biopsy, toxic megacolon, or pseudo- membranous colitis. Common fndings • Solitary flling defect: polyps are classifed according to histology. Also found are adenocarcinoma (i risk in ulcerative colitis, polyposis syndromes, villous adenoma) and less commonly metastases and lymphoma. Colonoscopy Remains a complementary technique and has the advantage of being both therapeutic and diagnostic (e. In elderly patients, Ct with prior bowel preparation and air insufation is less invasive and less arduous. Virtual colonoscopy Helical Ct images of distended colon taken during a breath-hold are used to obtain 2D or 3D images of the colon. Images are acquired in the supine and prone positions to assess lesional mobility (and thus distinguish stool from polyps). Computed tomographic virtual colonoscopy to screen for colorectal neoplasia in asymptomatic adults. Intravenous urogram this provides a good overview of the urinary tract and, in particular, the pelvicalyceal anatomy. An increasingly dense delayed nephrogram is seen in acute obstruction, acute hypotension, AtN, and renal vein thrombosis.
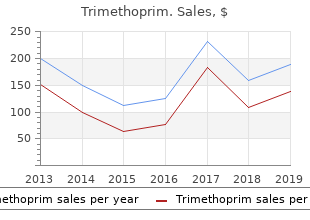
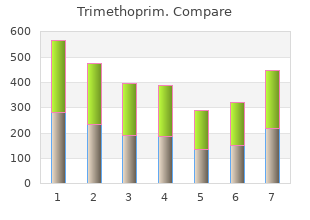
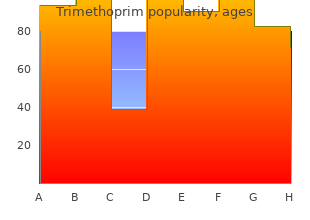
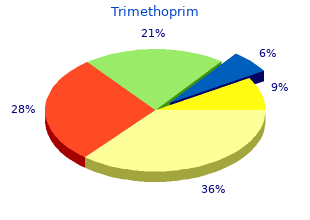
Despite differences in test accuracy and methodology purchase 480mg trimethoprim otc infection 3 metropolis collapse, virtually all evaluations can establish a baseline and be used to track relative progress during exercise training trimethoprim 480mg mastercard bacteria quiz. These equations produce a single expected aerobic capacity value for comparison to a measured response as opposed to percentiles discount 480 mg trimethoprim fast delivery antibiotic treatment for diverticulitis. Muscular strength refers to the muscle’s ability to exert a maximal force on one occasion purchase trimethoprim 960mg with amex yeast infection 8 weeks pregnant, muscular endurance is the muscle’s ability to continue to perform successive exertions or repetitions against a submaximal load, and muscular power is the muscle’s ability to exert force per unit of time (i. Traditionally, tests allowing few (≤3) repetitions of a task prior to reaching muscular fatigue have been considered strength measures, whereas those in which numerous repetitions (>12) are performed prior to muscular fatigue were considered measures of muscular endurance. Rationale Physical fitness tests of muscular strength and muscular endurance before commencing exercise training or as part of a health/fitness screening evaluation can provide valuable information on a client’s baseline physical fitness level. For example, muscular fitness test results can be compared to established standards and can be helpful in identifying weaknesses in certain muscle groups or muscle imbalances that could be targeted in exercise training programs. The information obtained during baseline muscular fitness assessments can also serve as a basis for designing individualized exercise training programs. An equally useful application of physical fitness testing is to show a client’s progressive improvements over time as a result of the training program and thus provide feedback that is often beneficial in promoting long-term exercise adherence. Results of any one test are specific to the procedures used, and no single test exists for evaluating total body muscular endurance or strength. Moreover, a warm-up consisting of 5–10 min of light intensity aerobic exercise (i. These warm-up activities increase muscle temperature and localized blood flow and promote appropriate cardiovascular responses for exercise. In both cases, caution must be used in the interpretation of the scores because the norms may not include a representative sample of the individual being measured, a standardized protocol may be absent, or the exact test being used (e. In addition, the biomechanics for a given resistance exercise may differ significantly when using equipment from different manufacturers, further impacting generalizability. Muscular Strength Although muscular strength refers to the external force (properly expressed in newtons, although kilograms and pounds are commonly used as well) that can be generated by a specific muscle or muscle group, it is commonly expressed in terms of resistance met or overcome. Static or isometric strength can be measured conveniently using a variety of devices including cable tensiometers and handgrip dynamometers. Measures of static strength are specific to the muscle group and joint angle involved in testing and thus may be limited in describing overall muscular strength. Despite this limitation, simple measurements such as handgrip strength have predicted mortality and functional status in older individuals (99,109). Adjust the grip bar so the second joint of the fingers fits snugly under the handle and takes the weight of the instrument. The subject holds the handgrip dynamometer in line with the forearm at the level of the thigh, away from the body. The subject squeezes the handgrip dynamometer as hard as possible without holding the breath (to avoid the Valsalva maneuver). Neither the hand nor the handgrip dynamometer should touch the body or any other object. The score is the highest of the two readings (to the nearest kilogram) for each hand added together. Norms based on resistance lifted divided by body mass for the bench press and leg press are provided in Tables 4. Free weights and other brands of resistance exercise machines which are more commonly used today may not provide the same weight–press ratio and to date have not been validated (54). Select an initial weight that is within the subject’s perceived capacity (~50%–70% of capacity). Such devices measure peak rotational force or torque, but an important drawback is that this equipment is substantially more expensive compared to other strength testing modalities (39). If the total number of repetitions at a given amount of resistance is measured, the result is termed absolute muscular endurance. A simple field test such as the maximum number of push-ups that can be performed without rest may be used to evaluate the endurance of upper body muscles (18). Previous editions of this publication included the curl-up (crunch) test as a simple field test for the measurement of muscular endurance. This edition of the Guidelines does not include the curl-up test in light of recent research suggesting that the test may not be sensitive enough to grade performance and may cause lower back injury (77,78,107). The push-up test is administered with men starting in the standard “down” position (hands pointing forward and under the shoulder, back straight, head up, using the toes as the pivotal point) and women in the modified “knee push-up” position (legs together, lower leg in contact with mat with ankles plantar-flexed, back straight, hands shoulder width apart, head up, using the knees as the pivotal point). The client/patient must raise the body by straightening the elbows and return to the “down” position, until the chin touches the mat. For both men and women, the subject’s back must be straight at all times, and the subject must push up to a straight arm position. The maximal number of push-ups performed consecutively without rest is counted as the score. The test is stopped when the client strains forcibly or unable to maintain the appropriate technique within two repetitions. Flexibility depends on a number of specific variables including distensibility of the joint capsule, adequate warm-up, and muscle viscosity. Just as muscular strength and endurance is specific to the muscles involved, flexibility is joint specific; therefore, no single flexibility test can be used to evaluate total body flexibility. Common devices for this purpose include goniometers, electrogoniometers, the Leighton flexometer, inclinometers, and tape measures. Comprehensive instructions are available for the evaluation of flexibility of most anatomic joints (21,87). These estimates can include neck and trunk flexibility, hip flexibility, lower extremity flexibility, shoulder flexibility, and postural assessment. Accurate measurements require in-depth knowledge of bone, muscle, and joint anatomy as well as experience in administering the evaluation. The sit-and-reach test has been used commonly to assess low back and hamstring flexibility; however, its relationship to predict the incidence of low back pain is limited (48). The sit-and-reach test is suggested to be a better measure of hamstring flexibility than low back flexibility (47). The relative importance of hamstring flexibility to activities of daily living and sports performance, therefore, supports the inclusion of the sit-and-reach test for health-related fitness testing until a criterion measure evaluation of low back flexibility is available. Although limb and torso length disparity may impact sit- and-reach scoring, modified testing that establishes an individual zero point for each participant has not enhanced the predictive index for low back flexibility or low back pain (15,46,80). Poor lower back and hip flexibility, in conjunction with poor abdominal strength and endurance or other causative factors, may contribute to development of muscular low back pain; however, this hypothesis remains to be substantiated (36). Normative data for the Canadian Trunk Forward Flexion test are presented in Table 4. It is also recommended that the participant refrain from fast, jerky movements, which may increase the possibility of an injury. The client sits without shoes and the soles of the feet flat against a sit-and- reach box with the zero mark at the 26 cm. The client should slowly reach forward with both hands as far as possible, holding this position approximately 2 s.
The blade is opening inserted in the normal way 480mg trimethoprim antimicrobial yarn, and if the view is obscured cheap 960 mg trimethoprim with visa p11-002 - antibioticantimycotic solution, • relative reduction in the distensible area below the the tip can be fexed so that it further elevates the vallecula foor of mouth (e generic 480 mg trimethoprim mastercard bacterial vaginosis home remedies. Curved blades are designed for the laryngoscope blade is made of multiple sections joined tip to be inserted into the vallecula with the standard together generic trimethoprim 480 mg antibiotics for uti nitrofurantoin, which in its ‘unfexed’ position resembles a Mac- Macintosh blade being inserted to the right of the tongue, intosh blade. Deployment of a lever after insertion of the while displacing it to the left side, whereas the straight blade fexes the whole length of the blade drawing the tip blade may be inserted posterior to the epiglottis and is upwards in a similar manner to the McCoy blade. There particularly useful for small children and adults with a are limited, but mostly positive, evaluations. Different laryngoscope blades require different tech- Rigid optical laryngoscopes niques for viewing the larynx, which must be learnt and used to maximize utility of that device. For example, the Fibreoptic technology dates back to the 1950s and is Henderson blade (Karl Storz, Germany), a modifcation of described in greater detail below under fexible fbreoptic the Miller blade, is a long straight blade with a ‘C’-shaped laryngoscopes. However, these benefts of the rigid optical laryngoscopes are all only of value if the laryngoscope design reliably facilitates and achieves tracheal intubation. Problems with rigid optical laryngoscopes stem from: • large numbers of devices with limited proof of effcacy • potential diffculty in achieving tracheal intubation despite a good view of the larynx, a common fnding which may be caused by a mismatch between where the device views as opposed to where it steers a Figure 6. In recent years a reduction in to achieve intubation the costs and size of the components, allied with improve- • trauma to unsighted areas in the airway during ments in video technology, has led to a profusion of new passage of tracheal tubes (and stylets) entrants to the market. Image transmission in this class of • increased cost, a very major issue with many devices device may be by fbreoptics, lenses/prisms/mirrors, or costing in excess of £5000 ($7000), often with increasingly, electronically from a distally mounted mini- disposable components also required. Throat specialists with head mounted and hand-held While rigid optical laryngoscopes have much potential, mirrors) at present the majority of devices are of unproven • the ability to retract tissues and make a space to look beneft, in both routine and diffcult cases. Much of the into or beyond (which fexible endoscopes can not do) research that has been performed on these devices is of • the ability to gain a view of the larynx with less 103 poor quality with extrapolation of results from easy mouth opening patients to diffcult patients, use of intermediate endpoints • reduced force and distortion of tissues leading to: and an emphasis on cohort rather than comparative reduced cardiovascular stimulation studies. They are • technical – a larger, brighter, higher-resolution image also principally limited to orotracheal intubation. As with many of these devices there is no This device was for many years the ‘standard’ for this group use of fbreoptics. It is one of the most popular of the but has to a large degree now been superseded. Originally the device was fully reus- broadly curved blade and uses fbreoptics to transmit the able after sterilization, but recently a newer version, the image from the tip to the eyepiece. It is designed to elevate ‘GlideScope Cobalt’, has been introduced with a reusable the jaw without the need for neck extension and for use fexible video baton which inserts into a disposable in patients with limited mouth opening. There are four different sized incorporated in later models to carry the tracheal tube handles in the reusable range (two sizes of a different (Fig. Like many bladed rigid ergonomically engineered, bladed, rigid video laryngo- optical laryngoscopes there is a danger of ‘easy view, dif- scope with an integral pivoting screen and detachable fcult intubation’, particularly if the manufacturer’s instruc- metal CameraStick. After various descriptions of use of clear plastic covers the CameraStick and is curved with a stylets with varying degrees of bend the manufacturers mid-portion angulation (Fig. At present there is have introduced specifc single-use tubes (GlideRite) and only an adult size; a ratchet mechanism at the base of the a dedicated stylet (Fig. A technique that involves device enables a 3 point retraction of the camera part for introduction of the styletted tube from the side of the use in smaller patients. It is operated by standard batteries, patient’s mouth towards the pharynx followed by 90° with a good battery life. Case reports have shown its utility rotation into the feld of view is described; as much of 185 Ward’s Anaesthetic Equipment Figure 6. A single-use plastic blade is copy while the instructor observes or directs progress from mounted on this and incorporates conduits for both the the remote monitor. The device is designed ing in direct laryngoscopy and use of the camera capability to be used in the midline and the tip rotated 90° anteriorly improves visualization of the larynx when compared to on entering the pharynx. It is likely to of image and light-carrying fbreoptics with integral optical have the same limitations, regarding tube choice, as the connections for the detachable light source and camera Airtraq (see below). Note the extreme curvature of the C-Mac ‘D’ blade (on top), for diffcult laryngoscopy, which cannot be used for direct laryngoscopy, see text. The size of the distal viewing lens explains why fbreoptic devices are so be attached and the image viewed on a remote screen con- easily foiled by secretions. Further designs attempt to assist nasal intubations and Airtraq double lumen tracheal tube insertion. First the conduit increases the bulk of user looks into a viewfnder where a series of prisms and the ‘blade’ and may increase the required mouth opening mirrors deliver an illuminated image from the tip of the compared to simpler bladed devices. A camera may different tracheal tube types and sizes will likely alter the 187 Ward’s Anaesthetic Equipment Figure 6. It has been shown for the Airtraq that use of tracheal tubes that are both preformed and whose external diameter is only a little smaller than the internal dimension of the conduit facilitate intu- bation; conversely, relatively small and non-preformed tracheal tubes will fail to adopt the shape of the conduit and therefore exit in a more posterior direction leading to a tendency for failure or oesophageal intubation. Disadvantages include an up to the tracheal tube should be simple and reliably achieved. The epiglottic elevator is modifed in design (a hole in the Optical stylets centre of it enables a view beyond) and colour (it is white, to minimize interference with images). After the device is Optical stylets are preformed rigid or malleable metal inserted a battery powered, low-defnition screen is attached guides containing an optical system (usually fbreoptics) to the connector to display an image. Three sizes cheal tube is loaded onto the stylet, which is then intro- of device are available, covering adults of 30 to 100 kg. While the stylet may be introduced into the trachea this should be avoided, altogether or limited to a small distance to avoid trauma. Oxygen can be insuffated during use, via an attachment for the tracheal tube, in the majority of stylets. It is designed to be introduced from the side of the mouth in a ‘retromolar approach’ using the non-dominant hand to elevate the jaw SensaScope and tongue. There There is limited published experience with the Bonfls is limited, largely positive evaluation of it. In the light of (Clarus Medical, as before) is a similar slightly shorter the arrival of the Ambu aScope (v. Both devices have somewhat greater video stylet will probably precede this publication. Murphy114 who, in • Requires time to learn and skill to use 1967, reported using the newly invented choledochoscope • Cost and necessity for decontamination may limit for intubation of the trachea. The by external diameter of fbrescope (and must be terms fexible intubating fbrescope, endoscope, scope, selected at start of procedure) bronchoscope, laryngoscope, and even tracheoscope are • Passage of tracheal tube over fbrescope is blind, used interchangeably with varying degrees of precision. Here we use the term fex- ineffective even in skilled hands ible fbrescope or scope to describe any suitable device, • Use in airway obstruction may worsen situation due and fexible endoscope to include also devices not using to ‘cork-in-bottle’ effect in awake patients fbreoptics but video technology for image transmission • Diffculty in sterilization may pose risk of transmission (see below). The manoeuvrability of a fexible endoscope means that it can be made to follow virtually any anatomical space and return an image from its tip. Because it presumes no Flexible fbreoptic laryngoscopes particular anatomical arrangement (i. Each fbre false assumption that the technique is the solution to all consists of a central glass core surrounded by a thin clad- airway diffculties: this is patently not so. However, the ding of another type of glass with a different refractive versatility and clinical utility of fexible endoscopes make index to that of the core glass. As a result of the difference them tools with everyday applications which all anaesthet- in refractive indices at the interface of the two materials, ists should be encouraged to master. For the purpose of transmitting illumination, the Advantages: arrangement of the fbres is unimportant, but for image • Primarily, the ability to see round more than one transmission the arrangement of the fbres relative to one corner due to unparalleled fexibility and another must be identical at either end of the bundle, as manoeuvrability each fbre carries a tiny portion of the overall image (in • Clinical utility: may be used in a very wide variety of the same way that many small dots make up the printed clinical circumstances image in a newspaper): this is called a coherent bundle.
Purchase 480mg trimethoprim with visa. Deploying artificial genes to overcome antibiotic resistance | Logan Collins | TEDxMileHigh.
The double-bundle reconstruction demonstrated increased resist- ance to posterior translation compared with the single-bundle reconstruction discount 960 mg trimethoprim fast delivery antimicrobial activity. If there is excessive excursion of the tendon cheap 480 mg trimethoprim antibiotics herpes, move the wire/drill bit and re- check generic trimethoprim 480mg online infection elite cme. Position knee in approximately 30° of fexion during fxation with slight varus force applied to knee cheap 480 mg trimethoprim with visa antibiotics for sinus infection levaquin. Step 3: Allograft Reconstruction Semimembranous • Variety of allografts can be used for this technique. Review article characterizing the anatomy of the medial side of the knee and outlining diagnostic and treatment strategies. The feet are passively externally ro- tated and the thigh-foot angle is measured and compared side to side. More than 15° of increased external rotation indicates a clinically signifcant injury. All • Popliteus tendon extremities must be well padded, including the contralateral leg (especially if the patient is in • Popliteofbular ligament the lateral decubitus position). For this reason, • Capsule and capsular thickenings the use of an arthroscopic knee holder is usually not recommended. This window exposes popliteus tendon, popliteofbular arthroscopic fuid egress and reduce the risk of iatrogenic compartment syndrome. Note that the inferior aspect of the lateral meniscus can be visualized through the capsular injury. In chronic cases or • The lateral meniscus can be visualized and repaired with suture to the lateral capsule when there is signifcant soft-tissue damage, or with suture anchors. Note that the graft is “fxed” wherever the leading edge of the washer or staple se- • Be careful not to violate the articular surface when placing suture anchors for meniscus/ cures the graft. Intraoperative fuoroscopy • If the whip-stitch causes the end of the graft to is helpful here. Step 5: Graft Passage • The two grafts are passed through the fbular and tibial tunnels respectively using the passing suture or wire (Fig. Extreme care must be taken to protect the peroneal nerve during graft passage and ensure that the graft does not pass around the nerve. The anterior limb of the graft is taken to the posterior side of the femoral guide-pin and the posterior limb is taken to the anterior side. The femoral pin should be repositioned if there is excessive excursion within the grafts. Step 6: Graft Fixation • The Muller (tibial) graft is fxed in the tibial tunnel with a bioabsorbable interference screw placed anteriorly. This position is selected because the spiked washer will trap the grafts distally at the approximate location of the guide-pin. The tibial graft should pass anteriorly as well and be pulled all the way around the screw. Step 7: Verification of reconstruction • Take the knee from full extension to full fexion to ensure fuid range of motion without excessive stress on the grafts. Note the femoral screw and soft-tissue washer will appear proud radiographically due to the interposed grafts. Step 2: Tibial and Fibular Tunnels • Prepared similarly to the previously described combined Larson fgure-of-8 and Muller popliteal bypass reconstruction technique. Encourage full extension to 90° of fexion by the end of the 2nd week postoperatively. A combined injury signifcantly increases posterior tibial transla- tion, varus displacement, and rotatory instability at the knee joint. Under clinician applied load, sectioning the lateral collateral ligament resulted in 2. Imaging Plain Radiographs • Identify direction of dislocation to formulate reduction plan and anticipated injury pattern. Stress Radiographs • Helpful to detect and quantify functional ligament defciency/instability. Single-stage surgery facilitates restoration of the central pivot of the knee and decreases stress on the collateral repair/reconstruction. Step 2: Tunnel Preparation and Graft Passage for Cruciate Ligament Reconstruction • Cruciate tunnels prepared frst. Step 3: Lateral and/or Medial Repair/Reconstruction • If multiple potentially converging tunnels are • Refer to the chapters on the respective procedures for more details. Step 4: Graft Fixation • Fix cruciate reconstruction on the other side of the joint to restore the central axis of the knee and normalize anatomical relationships on the medial/lateral side of the knee. Initially, no resistance is used and the seat is placed in a high position to prevent deep knee fexion. This is a review of knee dislocations that discusses the mechanism of injury and importance of early detection of associated vascular injury. The timing of surgical intervention is discussed along with special conditions that require delayed surgery. Controversies in the treatment of knee dislocations and multiligament reconstruction, J Am Acad Orthop Surg 17:197–206, 2009. Review of the evidence supporting treatment algorithms for multiligament knee injuries. Both groups were evaluated with subjective and objective scores and, although the differences were small, the acutely reconstructed group showed improved outcome. Popliteal magnetic resonance angi- ography was also performed on many of these patients and was found to have a 100% correlation with standard angiography. In one study, tears less than 10 mm in (or an extensor lag), although they may be able to maintain a straight leg raise in the width (as measured by ultrasound), treated setting of a high-grade partial thickness tear. Portals/Exposures • Make a midline incision starting at the superior pole of the patella and extending distally to the tibial tuberosity. Step 2 • Run an interlocking Krackow stitch using a #2 or #5 nonabsorbable suture. This will be helpful in determining the starting point for fexion during pain and arthrosis. This approach is especially useful in patients with poor tissue quality, systemic disease, or corticosteroid use. Step 7 • When patellar tendon tissue is defcient, • Close subcutaneous tissue in layers with 2-0 absorbable sutures, and the skin with consider reinforcement with autologous gracilis or semitendinosus tendon as described interrupted nylon sutures or staples. Step 2 • Run Krackow locking stitches using #2 nonabsorbable sutures on the medial and lateral aspects of the proximal and distal tendons, respectively (Fig. Step 3 • Tie the corresponding suture ends with the knee fexed at 30° and with the tendon ends approximated.
The pump should fit completely within the pocket without any part of the device extending beneath the incision cheap trimethoprim 960mg 11th antimicrobial workshop. There should be no tension on the sutures during closure of the incision or the wound is likely to dehisce buy cheap trimethoprim 480mg antibiotic resistance journal pdf. After pocket creation is completed buy trimethoprim 960 mg without prescription infection elite cme, a tunneling device is extended within the subcutaneous tissues between the paraspinous incision and the pocket (Fig buy 480mg trimethoprim bacteria 5utr. The catheter is then advanced through the tunnel (most tun- neling devices place a hollow plastic sleeve in the subcuta- neous tissue through which the catheter can be advanced from the patient’s back to the pump pocket). The catheter is then trimmed to a length that allows for a small loop of catheter to remain deep to the pump and attach to the pump. This loop allows for patient movement without placing tension on the distal catheter and causing it to be pulled from the thecal sac. Two or more sutures should be placed through the suture The catheter is secured to the paravertebral fascia using an loops or mesh enclosure surrounding the pump and used anchoring device supplied by the manufacturer. Newer anchors that secure the catheter directly without the need for the circumferential retaining sutures prevent the pump from rotating or flip- sutures around the anchor and catheter have been developed. A tunneling device provided by the manufacturer is used to A transverse incision is created in the abdominal wall midway position the catheter within the subcutaneous tissue between between the umbilicus and the anterior axillary line, and a the paravertebral incision and the abdominal pump pocket. In pocket of sufficient size is made to accommodate the pump large patients, the tunneling may require two segments: the using blunt dissection. The blunt dissection can be accom- first segment between the paravertebral incision and a small plished using the fingertips or by using surgical scissors and a transverse incision in the mid-axillary line and a second seg- repeated spreading (rather than cutting) motion. Chapter 15 Implantable Spinal Drug Delivery System Placement 215 Permanent Epidural Catheter Placement For placement of a permanent epidural catheter, patient positioning and use of fluoroscopy are similar to those described for intrathecal catheter placement. The interspace of entry will vary with the dermatomes that are to be cov- ered, particularly if local anesthetic solution is to be used. A typical loss-of-resistance technique is used to identify the epidural space, and a silastic catheter is threaded into the epidural space. A paraspinous incision is created, and the catheter is secured to the paraspinous fascia as described previously for intrathecal catheter placement. Two types of permanent epidural systems are available: a totally implanted system using a subcutaneous port that is accessed using a needle placed into the port through the skin and a percutaneous catheter that is tunneled subcu- taneously but exits the skin to be connected directly to an external infusion device. To place a permanent epidural with a subcutaneous port, a 6- to 8-cm transverse incision is made overlying the costal margin halfway between the xiphoid process and the anterior Figure 15-15. A pocket is created overlying the rib cage using After ensuring good hemostasis, the pump is placed within blunt dissection (Fig. The port must then be sutured securely to the fascia over in two layers: a series of interrupted subcutaneous sutures the rib cage. Care must be taken to ensure the port is secured to securely close the fascia overlying the pump and the catheter followed by a skin closure using suture or staples (Fig. The port is connected to The abdominal and paravertebral incisions are then closed in the epidural catheter and sutured to the fascia overlying the two layers: a layer of interrupted, absorbable suture within the inferior rib cage. The port must lie firmly in place over the ribs subcutaneous tissue overlying the pump and catheter, and a rather than the abdominal wall; without the support of the separate layer within the skin. This cuff should be placed about 1cm from the catheter’s exit site along the subcutaneous catheter track. The proximal and distal portions of the catheter are then trimmed, leav- ing enough catheter length to ensure there is no traction on the catheter with movement. The two ends of the catheter are connected using a stainless steel union supplied by the manufacturer and sutured securely. The paraspinous skin incision is then closed in two layers: a series of interrupted subcutaneous sutures to securely close the fascia overly- ing the catheter followed by a skin closure using suture or staples. The skin incision at the epidural catheter’s exit site in the right upper quadrant is closed around the base of the catheter using one or two simple, interrupted sutures. Complications Bleeding and infection are risks inherent to all open surgi- cal procedures. Bleeding within the pump pocket can lead to a hematoma surrounding the pump that may require Figure 15-18. Bleeding along the subcutaneous tunnel- Placement of a permanent percutaneous, tunneled epidural ing track often causes significant bruising in the region but catheter. Similar to other neuraxial tech- pieces: a distal, epidural portion and a proximal catheter length with a subcutaneous antibiotic-impregnated cuff and niques, bleeding within the epidural space can lead to sig- external access port. Signs of infection within the and dissection through a paravertebral incision, the proximal pump pocket typically occur within 10 to 14 days follow- catheter is tunneled from the costal margin to the paraverte- ing implantation but may occur at any time. Some practi- bral incision, and the catheter is pulled into the subcutaneous tioners have reported successful treatment of superficial tissues until the antibiotic-impregnated cuff lies 1 to 2 cm from the chest wall incision within the subcutaneous tissue. The infections of the area overlying the pocket with oral antibi- catheter segments are then trimmed, joined together using a otics aimed at the offending organism and close observation connector supplied by the manufacturer, and secured to the alone. The skin entry site on the chest wall is catheter’s subcutaneous course almost universally require secured around the exiting catheter using interrupted sutures. Catheter and deep tissue infections can extend to involve the neuraxis, result- firmly in a region that overlies the rib cage; if the port migrates ing in epidural abscess formation and/or meningitis. Perma- inferiorly to lie over the abdomen, it becomes difficult to nent epidural catheters without subcutaneous ports have a access. The rigid support of the rib cage holds the port firmly higher infection rate than those with ports in the first weeks from behind, allowing for easier access to the port. The skin after placement, but both systems have a similar, high rate incisions are then closed in two layers: a series of interrupted of infection when left in place for more than 6 to 8 weeks. This has led some practitioners to recom- To place a permanent epidural without a subcutaneous mend placing the catheter only in the awake patient so the port, a tunneling device is extended from the paraspinous patient can report paresthesiae during needle placement. Percutaneous in the midline at an interspace that is below the level of the epidural catheters are supplied in two parts: the proximal conus medullaris (L3/L4 or lower). Ensuring the size of the pocket is sufficient to prevent abdominal wall and connects with the distal portion of the tension on the suture line at the time of wound closure is catheter. The distal portion of the catheter is now secured essential to minimize the risk of dehiscence. Port migration to the tunneling device and pulled through the incision usually occurs because retaining sutures were omitted at the in the abdominal wall subcutaneously to emerge from the time of placement. Many catheters are sup- suture loops on the port and securely fastening them to plied with an antibiotic-impregnated cuff that is designed to the abdominal fascia will minimize the risk of migration. Chapter 15 Implantable Spinal Drug Delivery System Placement 217 Main drug reservoir access port Side access port Pump rotor Catheter connector Catheter (attachment to pump) A B Figure 15-19. Fluoroscopy can be used to readily identify the drug reservoir access port during routine periodic refilling of the pump using the 22-gauge Huber-type (noncoring) needle supplied by the manufacturer. By taking two sequential radiographs separated by several minutes, fluoroscopy can also be used to assess proper rotation of the rollers around the rotor in the peristaltic pump, as their position will change if the rotor is moving. The side access port can be accessed with a 25-gauge needle; the side access port is specifically designed to prevent entry with the larger needle used for drug refills. Once the catheter has been cleared, radiographic contrast can be injected and the course of the catheter examined along its entire length to detect any dislodgement or leaks.