Fairmont State College. N. Murak, MD: "Order cheap Flutamide online no RX - Discount Flutamide online".
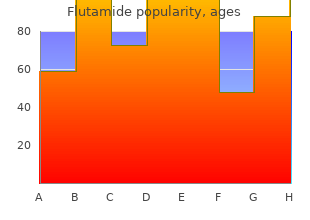
This technique results in a high rate of fracture union cheap flutamide 250 mg on line symptoms high blood sugar, promoted by the implant load-sharing characteristics with a modulus of elasticity that is close to bone cheap 250mg flutamide otc symptoms liver cancer, thereby avoiding stress shielding buy cheap flutamide 250 mg line in treatment 2. The flexible nailing technique for treatment of femur fractures in children also avoids the risk of avascular necrosis of the femoral head because of a more distal entry point on the bone generic 250mg flutamide mastercard medications causing pancreatitis, compared to standard rigid intramedullary nails that enter the medullary canal at the base of the femoral neck, where the primary vascular supply to the femoral head is located. The child is placed supine on a radiolucent operating table, although some surgeons prefer to use a fracture table when treating femur fractures with this method. The surgeon performs a closed reduction of the fracture with fluoroscopy assistance, proceeding to an open incision and reduction only if an acceptable fracture reduction cannot be achieved with closed techniques. After the fracture is aligned, a small incision for each nail is made on the extremity proximal to the physis at the knee. A drill is used to create an entry point in the cortex of the bone, and each nail is contoured before insertion through this entry point. The rare need for cast application is judged by intraop imaging for rotational and angular stability. A: Nail entry site through greater trochanter (antegrade) or distal metaphysic (retrograde). Vrsansky P, Bourdelat D, Al Faour: Flexible stable intramedullary pinning technique in the treatment of pediatric fractures. A plate and screws are commonly used, but an external fixator and/or spica cast may be placed instead. The usual surgical approach is direct lateral over the proximal shaft of the femur, beginning at the greater trochanter. The deep fascia is split, and the underlying vastus muscle is elevated subperiosteally to expose the femoral shaft. Normally, a power saw is used to make the osteotomy, and depending on the correction desired, a variety of internal fixation devices can be used. A 1- to 4-cm segment of femur may be removed in cases of superior hip dislocation to allow soft tissue relaxation and descent of the femoral head into the socket. Most proximal femoral osteotomies are performed in the subtrochanteric area, but some are performed in the intertrochanteric or base of the neck (Kramer compensating). The Southwick osteotomy is a more complicated example of a subtrochanteric osteotomy, which corrects for three directions (varus, lateral rotation, and extension). Koyonos L, Slenker N, Cohen S: Complications in brief: Osteotomy for lower extremity malalignment. The timing of the procedure is critical, based on the child’s bone age and discrepancy, which are plotted on a graph or computer program. The procedure is most commonly performed through small incisions (1”) above the knee, centered on the growth plate (physis) of the distal femur or proximal tibia. The bone block is rotated 90° or 180° and reinserted, causing a bony bridge across the physis. Blount subsequently used stout, reinforced staples to bracket the physis and “lock it. More recently, a percutaneous technique of simply drilling directly across the cartilaginous physeal growth plate, causing a bony bridge, has been used. Phemister method of epiphysiodesis (block of bone reversed, then reinserted to form osseous bar). Kemnitz S, Moens P, Fabry G: Percutaneous epiphysiodesis for leg length discrepancy. The procedure involves exposure of at least one end and a varying amount of the bony shaft. If the deformity is severe, the entire shaft is exposed via a longitudinal incision, usually laterally. The bone is divided (osteotomized) into the minimum number of segments that will allow a straight intramedullary rod to traverse the segments (usually 2–4 osteotomies). Variant procedure or approaches: Because a growing bone will elongate beyond the end of a simple intramedullary rod after 1–2 yr, the resulting unsupported portion of the bone will be liable to fracture or develop a new deformity. To obviate this problem, Bailey and Dubow developed an elongating rod system, consisting of an outer tubular rod sleeve (the female portion) and an inner obturator portion (male). The system elongates much like a car radio antenna and decreases the need for frequent revisions. The surgical technique is, however, identical to any fragmentation rodding, except that both ends of the bone must be exposed. Lesser discrepancies are dealt with by bone shortening or epiphysiodesis of the long side. The basic principles include (a) application of an adjustable, external fixator; (b) “low-energy,” transverse bone cut (osteotomy without use of a power saw) through a small, longitudinal incision over the involved bone; (c) preservation of the periosteal sleeve; (d) gradual lengthening, usually 1 mm/day in fractional adjustments; and (e) when the desired limb length is obtained, either use bone graft and plate acutely or leave until the bone gap fills in and stabilizes (average 38 d/cm gained). Limb lengthening dates back to the early 1900s, but it fell into disfavor because of the high rate of major complications. Wagner improved the technique by introducing a simplified, unilateral, large-pin fixator, but performed the osteotomy in the midshaft and began lengthening immediately (Fig. This technique usually requires a bone graft and later plating as a second operation to obtain healing. DeBastiani uses a similar large-pin fixator (Orthofix) but performs the osteotomy more toward the end of the bone (metaphysis) and waits a week before beginning the lengthening. Ilizarov introduced a more complex, but more adaptable, small-pin transfixation system with a circular fixator. In a similar fashion, the Ilizarov method stretches the healing callus (callotasis). Aronson J: Limb-lengthening, skeletal reconstruction, and bone transport with the Ilizarov method. These disorders include a spectrum of malalignments of the patella, ranging from simple excess lateral tilt, recurrent partial subluxation, and recurrent episodic dislocation, to irreducible chronic dislocation. As such, the surgical procedures also encompass a spectrum of complexities, depending on the degree of instability. Proximal realignment includes (a) lateral release, which is the division of the contracted lateral patellar retinacular joint capsule and other tight lateral tissue—the first step in all surgical repair; (b) medial tightening, including reefing and/or advancement of the medial capsule and vastus medialis muscle insertion; and (c) distal realignment, consisting of redirection of the patellar tendon more medially (and sometimes more anteriorly). Variant procedure or approaches: Arthroscopic or open lateral release is the simplest and first-step procedure. It may be sufficient when there is only subluxation and not true dislocation, and it has the advantage of being an outpatient procedure. For frank dislocation, an open “proximal realignment” also includes the medial tautening. If this is not sufficient to hold the patella centralized and if the patient has open epiphyses (< 16 yr), the lateral half of the patellar tendon may be released (distal realignment) and reattached medially (Roux-Goldthwait) or the patella may be held medially by tenodesing the semitendinosus tendon to it. In skeletally mature patients, the bony insertion of the patellar tendon is osteotomized and transferred medially (Trillat) or anteriomedially (Maquet). The Hauser procedure of distal and medial transfer of the tibial tubercle has had a very poor long-term outcome and is seldom performed. Hennrikus W, Pylawka T: Patellofemoral instability in skeletally immature athletes. Nelitz M, Dreyhaupt J, Reichel H, Woelfle J, Lippacher S: Anatomic reconstruction of the medial patellofemoral ligament in children and adolescents with open growth plates: surgical technique and clinical outcome. Originally used for the treatment of poliomyelitis sequelae, these lengthenings and transfers are now used for a variety of deformities 2° more common neuromuscular disorders, such as cerebral palsy, muscular dystrophies, Charcot-Marie-Tooth disease, and traumatic nerve palsies.
Diseases
- Multiple joint dislocations metaphyseal dysplasia
- Bejel
- Nemaline myopathy, type 2
- Anti-HLA hyperimmunization
- Grix Blankenship Peterson syndrome
- Hyperhomocysteinemia
Prospective comparison of valve regurgitation quantitation by cardiac magnetic resonance imaging and transthoracic echocardiography purchase flutamide 250 mg online treatment emergent adverse event. Eligibility and disqualification recommendations for competitive athletes with cardiovascular abnormalities generic flutamide 250 mg on line treatment 8th february. Task Force 5: Valvular Heart Disease: a scientific statement from the American Heart Association and American College of Cardiology generic flutamide 250mg free shipping symptoms lung cancer. Prospective validation of the prognostic usefulness of B-type natriuretic peptide in asymptomatic patients with chronic severe aortic regurgitation buy discount flutamide 250 mg on line treatment hepatitis c. Speckle-tracking echocardiography for predicting outcome in chronic aortic regurgitation during conservative management and after surgery. The impact of renin-angiotensin-aldosterone system blockade on heart failure outcomes and mortality in patients identified to have aortic regurgitation: a large population cohort study. Effect of beta-blocker therapy on survival in patients with severe aortic regurgitation results from a cohort of 756 patients. Improved outcomes after aortic valve surgery for chronic aortic regurgitation with severe left ventricular dysfunction. Surgery for aortic dilatation in patients with bicuspid aortic valves: a statement of clarification from the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Toward predictable repair of regurgitant aortic valves: a systematic morphology-directed approach to bicommissural repair. Valve configuration determines long-term results after repair of the bicuspid aortic valve. Repair of the regurgitant bicuspid or tricuspid aortic valve: background, principles, and outcomes. Transcatheter aortic valve implantation for pure severe native aortic valve regurgitation. Usefulness of bicuspid aortic valve phenotype to predict elastic properties of the ascending aorta. Bicuspid aortic valves with different spatial orientations of the leaflets are distinct etiological entities. Aortic dilatation patterns and rates in adults with bicuspid aortic valves: a comparative study with Marfan syndrome and degenerative aortopathy. Bicuspid aortic cusp fusion morphology alters aortic three-dimensional outflow patterns, wall shear stress, and expression of aortopathy. The bicuspid aortic valve: an integrated phenotypic classification of leaflet morphology and aortic root shape. Natural history of asymptomatic patients with normally functioning or minimally dysfunctional bicuspid aortic valve in the community. Type A aortic dissection in patients with bicuspid aortic valves: clinical and pathological comparison with tricuspid aortic valves. The interval between the initial episode of rheumatic fever (see Chapter 74) and clinical evidence of mitral valve obstruction is variable, ranging from a few years to more than 20 years. Rheumatic fever results in characteristic changes of the mitral valve; diagnostic features are thickening 2 at the leaflet edges, fusion of the commissures, and chordal shortening and fusion (Fig. With acute rheumatic fever, the changes include inflammation and edema of the leaflets, with small fibrin-platelet thrombi along the leaflet contact zones. Subsequent scarring leads to the characteristic valve deformity, with obliteration of the normal leaflet architecture by fibrosis, neovascularization, and increased collagen and tissue cellularity. Aschoff bodies, the pathologic hallmark of rheumatic disease, are seen most frequently in the myocardium, not the valve tissue, with Aschoff bodies identified in only 2% of autopsied patients with chronic valve disease. Note the commissural fusion that results in doming of the leaflets in the long-axis view and in a decrease in the width of the mitral orifice in the short-axis view. The patient has relatively thin, flexible leaflets with little subvalvular involvement. In earlier stages of the disease, the relatively flexible leaflets snap open in diastole into a curved shape because of restriction of motion at the leaflet tips (see Fig. The symmetric fusion of the commissures results in a small, central oval orifice in diastole that on pathologic specimens is shaped like a fish mouth or buttonhole because the anterior leaflet is not in the physiologic open position (Fig. Commissural fusion leaves the mitral valve with a small, circular orifice that has been likened to a fish mouth. In North America and Europe, with approximately 1 case per 100,000 population, patients present with severe valve obstruction in the sixth decade of life. By contrast, in Africa, with a disease prevalence of 35 per 100,000, severe disease often is seen in teenagers. Conversely, evidence favoring superimposed calcific valve disease is the observation that restenosis after mitral valvuloplasty is caused by leaflet thickening and fibrosis, rather than representing 3 recurrent commissural fusion. Mitral annular calcification 5 often develops in patients with calcific aortic valve disease. Characterized by heavy calcification and 6 7 thickening of the aortomitral curtain, it often requires multimodality imaging for full characterization. Pathophysiology The most useful descriptor of the severity of mitral valve obstruction is the degree of valve opening in diastole, or the mitral valve orifice area. Thus a doubling of flow rate quadruples the pressure gradient, and any further reduction in valve area only exacerbates this. Because diastole shortens proportionately more than systole as heart rate increases, the time available for flow across the mitral valve is reduced at higher heart rates. It also accounts for the equally rapid clinical improvement in these patients when the ventricular rate is slowed. These changes in the pulmonary vascular bed may also exert a protective effect; the elevated precapillary resistance makes the development of symptoms of pulmonary congestion less likely by tending to prevent blood from surging into the pulmonary capillary bed and damming up behind the stenotic mitral valve. In these patients, symptoms are caused by a low cardiac output rather than by pulmonary congestion. These patients frequently have resting weakness and fatigue secondary to a low cardiac output, with low-output and pulmonary congestion symptoms with exercise. These changes lead to disparate conduction velocities and inhomogeneous refractory periods. Symptoms may be caused by a reduced ability to increase cardiac output normally with exercise or elevated pulmonary venous pressures and reduced pulmonary compliance. Vital capacity is reduced, presumably because of the presence of engorged pulmonary vessels and interstitial edema. Pulmonary edema may be caused by any condition that increases the flow rate across the stenotic mitral valve, either because of an increase in total cardiac output or a reduction in the time available for blood flow across the mitral orifice to occur. Usually, symptom status can be accurately assessed by a directed history, asking the patient to compare current levels of maximum exertion with those at specific times in the past. Interviewing the family may reveal limitations that the patient does not acknowledge. Exercise testing may be useful for selected patients to determine functional status objectively and may be combined with Doppler echocardiography (see later) to assess exercise hemodynamics. The pink, frothy sputum characteristic of acute pulmonary edema with rupture of alveolar capillaries also may develop in these patients.
Katuvira (Capsicum). Flutamide.
- Arthritis pain when applied to the skin.
- Cluster headache, when used nasally.
- Nerve pain (neuropathy) in people with diabetes when applied to the skin.
- Colic, cramps, toothache, blood clots, fever, nausea, high cholesterol, heart disease, stomach ulcers, heartburn, irritable bowel syndrome, migraine headache, allergic rhinitis, perennial rhinitis, nasal polyps, muscle spasms, laryngitis, swallowing dysfunction, and other conditions.
- Back pain.
- Dosing considerations for Capsicum.
- What other names is Capsicum known by?
- What is Capsicum?
- Are there safety concerns?
- Pain from shingles when applied to the skin.
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96908
Transcatheter approaches to tricuspid valve repair and replacement using various methods 31 buy 250mg flutamide free shipping symptoms kennel cough,32 and devices are feasible and currently being studied in clinical trials (see Chapter 72) discount 250 mg flutamide amex medicine cabinet with lights. The risk of thrombosis of mechanical prostheses is greater in the tricuspid than in the mitral or the aortic position buy cheap flutamide 250mg online treatment yeast overgrowth, presumably because pressure and flow rates are lower in the right side of the heart generic flutamide 250 mg without prescription severe withdrawal symptoms. For this reason, a bioprosthesis is the valve of choice for the tricuspid position in adults. However, management decisions should be made by a heart valve team, including cardiology, cardiac surgery, and infectious disease specialists. Diseased valvular tissue should be excised to eradicate the endocarditis, and antibiotic treatment can then be continued. A bioprosthetic valve may therefore be inserted several months after valve excision and control of the infection. Rheumatic inflammation of the pulmonic valve is very uncommon, usually is associated with involvement of other valves, and rarely leads to serious deformity. Carcinoid heart disease often involves the pulmonic valve, and plaques, similar to those involving the tricuspid valve, are often present in the outflow tract of the right ventricle of patients with malignant carcinoid. A, Zoomed two-dimensional parasternal short-axis image at the level of the aortic valve shows the pulmonic valve in long axis in mid-diastole, demonstrating a marked thickening with retraction of the pulmonic valve leaflets (arrow) and resulting in failure of leaflet closure. Pulmonic Regurgitation Causes and Pathology Pulmonic regurgitation can result from dilation of the valve ring secondary to pulmonary hypertension (of any cause) or from dilation of the pulmonary artery. These include congenital malformations, such as absent, malformed, fenestrated, or supernumerary leaflets. Less common causes include trauma; carcinoid syndrome, in which leaflet thickening and retraction result in mixed stenosis and regurgitation (see Fig. B, Doppler tracing shows a dense signal in diastole with a steep deceleration slope that reaches the baseline before the end of diastole (arrow). D, Graph of the pulmonary artery flow within the region of interest indicated in C demonstrates both antegrade and retrograde flow. The right ventricle is hyperdynamic and produces palpable systolic pulsations in the left parasternal area, and an enlarged pulmonary artery often produces systolic pulsations in the second left intercostal space. An S and S originating from the right ventricle often are audible, most readily in the3 4 fourth intercostal space at the left parasternal area, and are augmented by inspiration. This murmur is high-pitched, blowing, and decrescendo, beginning immediately after P , and is most prominent in the2 left parasternal region in the second to fourth intercostal spaces. Both the pulmonary artery and right ventricle are usually enlarged, but these signs are nonspecific. Abnormal motion of the septum characteristic of volume overload of the right ventricle in diastole and septal flutter may be evident. Additionally, the density of the Doppler profile of the jet is increased, and reversal of flow in the pulmonary artery by color flow imaging can be detected a distance from the valve. Multivalvular Disease Various clinical and hemodynamic syndromes can be produced by different combinations of valvular abnormalities. It frequently is caused by rheumatic fever but is also seen with congenital heart disease, carcinoid heart disease, radiation heart disease, and connective tissue disorders. Marfan syndrome and other connective tissue disorders may cause multivalve prolapse and dilation, resulting in multivalvular regurgitation. Congenital heart disease may predispose to infective endocarditis or degenerative disease. In patients with multivalvular disease, the clinical manifestations depend on the relative severity of each of the lesions. When the valvular abnormalities are of approximately equal severity, clinical manifestations produced by the more proximal (upstream) of the two valvular lesions (i. It is important to recognize multivalvular involvement preoperatively because failure to correct all significant valvular disease at the time of operation increases mortality. Specific guideline 13,40 recommendations exist for concomitant valve surgery in patients undergoing surgery on another valve. In patients with multivalvular disease, the relative severity of each lesion may be difficult to estimate by clinical examination because one lesion may mask the manifestations of the other. Therefore, patients with suspected multivalvular involvement being considered for surgical treatment should undergo careful clinical evaluation and full Doppler echocardiographic evaluation. Mixed stenotic and regurgitant lesions can be assessed with a combination of two- and three-dimensional imaging, including planimetry of stenotic orifices, color flow imaging, and Doppler. Multiple valves can be systematically assessed during 41 exercise; this is particularly helpful in assessing the patient with exertional symptoms, especially when these seem disproportionate to findings on imaging at rest. Rheumatic aortic valve disease may result in primary regurgitation, stenosis, or mixed stenosis and regurgitation. Echocardiography is of decisive value in the evaluation of patients with rheumatic disease and allows accurate diagnosis of the presence and severity of multivalve involvement, taking into consideration the altered flow conditions with serial lesions. It is vital to recognize the presence of hemodynamically significant aortic valvular disease (i. Physical findings may be confusing because it may be difficult to recognize two distinct systolic murmurs. When both valvular leaks are severe, this combination of lesions is poorly tolerated. With severe combined regurgitant lesions, regardless of the cause of the mitral lesion, blood may reflux from the aorta through both chambers of the left side of the heart into the pulmonary veins. An intrinsically normal mitral valve that is regurgitant because of a dilated annulus should not be replaced. Surgical Treatment of Multivalvular Disease Replacement or repair of multiple valves presently comprises 12% of valve procedures and usually is 43 associated with a higher risk and poorer survival than replacement of either of the valves alone. The operative risk of double-valve replacement is approximately 70% higher than for single-valve replacement. In view of the higher risks, a higher threshold is required for multivalvular versus single-valve surgery. Diagnosis and treatment of tricuspid valve disease: current and future perspectives. Evaluation of tricuspid valve morphology and function by transthoracic three-dimensional echocardiography. Trends and outcomes of tricuspid valve surgery in North America: an analysis of more than 50,000 patients from the Society of Thoracic Surgeons database. Right ventricular systolic function in organic mitral regurgitation: impact of biventricular impairment. Significant lead-induced tricuspid regurgitation is associated with poor prognosis at long-term follow-up. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Pathophysiology of tricuspid regurgitation: quantitative Doppler echocardiographic assessment of respiratory dependence. In vitro characterization of the mechanisms responsible for functional tricuspid regurgitation. Dynamics of the tricuspid valve annulus in normal and dilated right hearts: a three-dimensional transoesophageal echocardiography study.