Montana State University-Northern Havre. E. Keldron, MD: "Order cheap Indinavir online no RX - Effective Indinavir online OTC".
If shocked (poor peripheral pulses purchase 400 mg indinavir mastercard treatment alternatives, poor capillary filling with tachycardia order indinavir 400 mg with amex symptoms dizziness nausea, and/or hypotension) give 10 ml/kg 0 purchase 400 mg indinavir medications epilepsy. However indinavir 400mg with visa bad medicine 1, too rapid reduction in intravascular osmolality may aggravate the process. Proceed with urgency but with caution • Type of fluid : Initially use isotonic solution. Maintenance requirements Age 0-2 yrs 80 ml/kg/24 hrs Age 3-5 yrs 70 ml/kg/24 hrs Age 6-9 yrs 60 ml/kg/24 hrs Age 10-14 yrs 50 ml/kg/24 hrs Adult (>15) 30 ml/kg/24 hrs Add calculated maintenance (for 48 hrs) and estimated deficit, subtract the amount already given as resuscitation fluid, and give the total volume evenly over the 48 hours. Hourly rate is calculated as follows: 48 hr maintenance + deficit – resuscitation fluid already given 48 (In addition to clinical assessment of dehydration, calculation of effective osmolality may be valuable to guide fluid and electrolyte therapy. Because the severity of dehydration may be difficult to determine and is overestimated, infuse fluid each day at a rate rarely in excess of 1. Hypokalemia at presentation may be related to prolonged duration of disease, whereas hyperkalemia primarily results from reduced renal function. Start potassium replacement immediately if the patient is hypokalemic; otherwise, start potassium concurrent with starting insulin therapy. Phosphate Depletion of intracellular phosphate occurs and phosphate is lost as a result of osmotic diuresis. However, prospective studies have failed to show significant clinical benefit from phosphate replacement. Administration of insulin stops further ketoacid synthesis and allows excess ketoacids to be metabolized. Also, treatment of hypovolemia will improve decreased tissue perfusion and renal function, thus increasing the excretion of organic acids and reversing any lactic acidosis, which may account for 25% of the acidemia. In addition, alkali therapy may increase hepatic ketone production, thus slowing the rate of recovery from the ketosis. These findings, however, do not address the issue that there may be select patients who may benefit from cautious alkali therapy, including those with severe acidemia (arterial pH: <6. The signs and symptoms of cerebral edema include: • Headache and slowing of heart rate • Change in neurological status (restlessness, irritability, increased drowsiness, incontinence) • Specific neurological signs (e. Management of Cerebral Edema • Exclude hypoglycemia as a possible cause of any behavior change. In the initial 6-10 h, nothing should be given orally and gastric lavage may be necessary in the drowsy child who is vomiting. However, as soon as the child has recovered consciousness and can sit up and eat, he/she should be encouraged to do so. If suspected, every attempt should be made to identify the precipitating infection, which should then be aggressively treated using appropriate antibiotics. Clinical and laboratory features of type 1 diabetic children at the time of diagnosis. An approach to prevention of recurrent diabetic ketoacidosis in the pediatric population. The Pediatric Emergency Medicine Collaborative Research Committee of the American Academy of Pediatrics. European Society for Paediatric Endocrinology/ Lawson Wilkins Pediatric Endocrine Society Consensus Statement on Diabetic Ketoacidosis in Children and Adolescents. Low-dose insulin infusion in the treatment of diabetic ketoacidosis bolus versus no bolus. The use of an insulin bolus in low-dose insulin infusion for pediatric diabetic ketoacidosis. Comparative study of different insulin regimens in management of diabetic ketoacidosis. Oxygen availability from the blood and the effect of phosphate replacement on erythrocyte 2, 3-diphospho-glycerate and hemoglobin oxygen affinity in diabetic ketoacidosis. Prevention of hypophosphatemia by phosphate infusion during treatment of diabetic ketoacidosis and hyperosmolar coma. Potassium balance during treatment of diabetic ketoacidosis with special reference to the use of bicarbonate. Cerebral edema during treatment of diabetic ketoacidosis: are we any nearer finding a cause? Development of fatal cerebral edema during outpatient therapy for diabetic ketoacidosis. Factors associated with adverse outcomes in children with diabetic ketoacidosis-related cerebral edema. Frequent hypoglycemic episodes in the treatment of patients with diabetic ketoacidosis. A high index of suspicion is necessary to recognize an endocrine emergency; appropriate tests can then be arranged to reach the diagnosis. Hypoglycemia is not a diagnosis by itself but is a manifestation of a variety of metabolic and endocrine disorders. The serum or plasma level of blood glucose tends to be 12-15% higher than the whole blood glucose. Contrary to the general belief asymptomatic hypoglycemia is as dangerous as symptomatic variety and should be investigated and treated with the same seriousness as the symptomatic form. Etiology Etiology can broadly be divided into those caused by substrate deficiency such as malnutrition, malabsorption, poor hepatic stores, etc. Clinical Features Clinical features of hypoglycemia are usually non-specific especially in the neonatal period. In neonate these include, lethargy, jitteriness, apnea, cyanosis, respiratory distress, poor feeding, hypothermia, myoclonic jerks or convulsions. In older children adrenergic hormone release in response to hypoglycemia dominate the symptoms in the form of sweating, tremors, hunger, pallor, tachycardia and shakiness followed by symptoms of neuroglycopenia in the form of sleepiness, lethargy, visual difficulty, ataxia, behavioral abnormalities and frank convulsions or unconsciousness. In cases where hypoglycemia is prolonged and severe, permanent brain damage results. Amino acids and organic acids Approach to Diagnosis of Hypoglycemia Broadly speaking hypoglycemia can be divided into 2 categories: Ketotic and Non-Ketotic depending on the presence or absence of ketones in the serum and/or urine. Non-Ketotic hypoglycemia is usually caused by either hyperinsulinism or by an oxidation defect such as carnitine deficiency. Presence of hepatomegaly in Ketotic hypoglycemia suggests glycogen storage disease (such as glucose 6 phosphatase deficiency) and other metabolic defects and specific enzyme assays are necessary for the diagnosis. In the absence of hepatomegaly endocrine deficiencies such as growth hormone deficiency, adrenal failure and hypothyroidism should be suspected. Treatment Immediate management consists of intravenous bolus of 10% dextrose in a dose of 2-2. Blood glucose is checked after 5 minutes and if there is no improvement in the blood glucose concentration, another bolus of 10% dextrose is given. Hypertonic solutions like this can cause permanent brain damage and must be avoided.
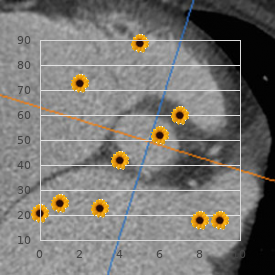
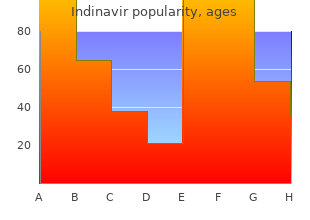
Residual volume is also determined by muscle strength (to overcome chest wall and lung recoil) and 400 mg indinavir sale when administering medications 001mg is equal to, in particular generic indinavir 400 mg line treatment lice, airway closure discount 400mg indinavir medicine 8 soundcloud. Periodicity of air ow limitation and symptoms are de ning careful buy 400 mg indinavir with amex treatment syphilis, detailed lung function assessments that include asthma characteristics and represent the periodic/e ervescent placement of an esophageal balloon, which is beyond the nature of the disease. Patients demonstrate marked variability capabilities of all but a few laboratories, the exact nature of the loss of lung function is largely a surmise. Bronchodilator responsiveness is generally less or about the same in patients with asthma. We have reported chial challenge tests, coupled with a careful history, results that the loss of central airway function as measured by in a clear picture of the disease process and its severity. Children with severe asthma in early life o en have reduced lung func- tion in adulthood that does not respond to bronchodila- tors. Lung function declines tic recoil such as seen in some asthmatics, patients with with age but it does so in a variable fashion. Surprisingly little is known about the variable in bronchitis or acute-status asthma. UpToDate Identi cation of asthma phenotypes using cluster in Pulm Disease and Critica Care. Peak ow monitoring in clinical prac- obstructive pulmonary disease phenotypes: the tice and clinical asthma trials. Lessons from structure-function in asthma: Physiological and morphological determinants of Myths and truths about what we teach. Frequency single-breath N2 test identify the smoker who will dependence of compliance as a test for obstruction in develop chronic air ow limitation? Peripheral tamine: Relationship to the late asthmatic response airways responsiveness to cool, dry air in normal and and change in airway caliber. Interaction Bronchodilator reversibility testing in chronic between parenchyma and airways in chronic obstructive pulmonary disease. Factors and overlap syndrome: A longitudinal study in young associated with bronchial responsiveness to his- European adults. Guide to the evaluation of pulmonary ological, and radiological features of asthma- function. Early intervention of therapy ciation between childhood asthma and adult in asthma. Expiratory spirometry was consistent with moderate to severe obstruction with signifcant response to inhaled albuterol. Blood eosinophils were mildly elevated, and total IgE remained elevated consistent with Th2 eosinophilic asthma. There was a childhood history of allergic asthma that persisted into adulthood and despite treatment, he continued to experience limited exercise ability. Social history was remarkable for smoking, which began at age 18 with a cumulative smoking history of 42 pack years. Many patients with a history of chronic cigarette smoking have persistent expiratory airfow obstruction despite partial reversibility with therapeutic intervention. There may be variable expiratory airfow limitation and markers of Th2 eosinophilic infammation noted initially. This includes increased blood and/or sputum eosinophils, increased serum total IgE, and hyperresponsive airways. Orie and colleagues hypothesized during the First Bronchitis Symposium held in Groningen, Netherlands, in 1961, that the various forms of airway obstruction—such as asthma, chronic bronchitis, and emphysema—should 6. Increased oped progressive airway obstruction compared to smokers blood eosinophils, as a surrogate of sputum eosinophils, without recurrent infections. More recently, Postma and colleagues8 provided an in- e primary analysis did not show a di erence in acute depth analysis of the multiple endogenous and exogenous exacerbations. Kaufman, and Nadel identi ed the reversible loss of Furthermore, the reduction in lung elastic recoil pres- lung elastic recoil in acute asthma. Subsequently, it was sure [Pst(l)] is similar as to the reduction in intrinsic airway also noted that the persistent loss of lung elastic recoil in conductance (Gus). There was not only disorganization and unevenly distributed enlarged airspaces, but also disrupted alveolar septa even visible at this magni cation as previously reported. Fig 3e is control Case in 82-year-old asthmatic woman with reversible expiratory air ow limitation with treatment. Microscopic morphometry was consistent with “senile lung” with nearly homogenous acinar hyperin a- tion and alveolar ductal ectasia but without unevenly distributed airspace enlargement, septal disruption, with no free septal fragments detached from the surrounding structures. Long-term chronic bronchitis, asthma, and air ow obstruc- prognosis of asthma, chronic obstructive pulmonary tion: 25 years on from the Ciba symposium. Against the Dutch hypothesis: Asthma prognosis of asthma–chronic obstructive lung disease and chronic obstructive pulmonary disease are overlap. Sputum death in patients with asthma and asthma–chronic eosinophilia and the short term response to inhaled obstructive pulmonary disease overlap syndrome. Elastic recoil of the eosinophil counts, exacerbations, and response to the lungs in chronic asthmatic patients before and after addition of inhaled uticasone furoate to vilanterol in therapy. The static elastic proper- ease: A secondary analysis of data from two parallel ties of the lungs in asthma. Comparison with normal and emphy- Benralizumab for chronic obstructive pulmonary sematous lungs. De Magalhaes Simoes S, dos Santos M, da Silva of asthma and chronic obstructive pulmonary disease. The centrilobular form of Chronic obstructive pulmonary disease overlap syn- hypertrophic emphysema and its relation to chronic dromes. Epidermal growth fac- mild emphysema in nonsmoking patients with chronic tor receptor-mediated innate immune responses asthma with persistent airway obstruction. The patient had previously received short courses of broad-spectrum antibiotics and oral corticosteroids, which had only partially resolved his symptoms. His current drug treatment was an inhaled corticosteroid (400 mcg, once daily) in combination with a long-acting β -agonist and an inhaled short-acting2 β2-agonist (taken as required). His respiratory symptoms were not precipitated by exposure to allergens and there was no seasonal variability in his symptoms. Furthermore, the patient gave a 10-year history of a chronic cough associated with daily expectoration of mucoid sputum. He had been smoking for approximately 20 years, currently around 15 cigarettes per day. Both of his parents were lifelong cigarette smokers, and his wife was also a smoker. Higher rate of active smoking and exposure Predicted Measured short-acting β2-agonist to passive smoke are found in developing countries. Black Women’s Health ⚫ What are the prevalence rates for active and passive Study recently reported that a history of current or former tobacco smoke exposure in chronic airway disease? In the United States, however, a higher proportion of people with asthma smoke (21%) compared to Worldwide, more than 1 billion people are estimated to use the general population (16. In on Drug Use and Health between 2005 and 2013 found no 2014 the prevalence of current cigarette smoking among decline in cigarette smoking among people with asthma. In the United ing di ers in certain subgroups of asthma, with increased States, exposure to passive smoke has reduced by half since rates among people visiting emergency rooms with exacer- 2000.
Assess direct and consensual reflex in each eye in turn with the use of a pen torch cheap 400mg indinavir free shipping medicine river. Test accommodation by asking the patient to look into the distance and then focus on an object close to their face buy 400 mg indinavir with amex medications with codeine. Demonstrate the ‘red reflex’ by shining the light in each pupil and then examine each fundi purchase indinavir 400mg without a prescription symptoms quadriceps tendonitis, optic discs and macula indinavir 400mg with visa x medications. Ask the patient to follow your finger up and down, right (up and down) and then left (up and down). If present, ask the patient to close each eye in turn to identify the side of the false image. Assess convergence by asking the patient to focus on your finer as it is brought in from a distance towards the tip of their nose. Sensory function: Assess sensation (fine touch, temperature) in the three divisions (ophthalmic, maxillary, mandibular) and compare both sides of the face. Jaw jerk: Place your finger in the midline over the tip of the patient’s mandible, with the patient’s mouth slightly open. Ask the patient to raise their eyebrows, wrinkle forehead (frown), close their eyes, smile, show their teeth, blow out their cheeks and pucker their lips. Sensory function (taste): Test the anterior two-thirds of each side of the patient’s tongue (using sweet/salt, bitter/or sour). Perform Weber’s test (lateralizing sign) in each ear by placing a vibrating turning fork over the middle of the patient’s forehead. A normal response to cold water irrigation is for the patient to develop nystagmus towards the contralateral side. A normal response to warm water irrigation is for the patient to develop nystagmus towards the ipsilateral side. Assess tactile sensation of the tonsil, palate and upper pharynx with a tongue depressor. Assess strength on lateral deviation by asking the patient to move their tongue from side to side and then assess bulk and contraction strength. Visual fields – Stand 2 feet in front of the patient and ensure you are at eye level. Move your hands to side half way between yourself and the patient, wiggle fingers, ask the patient when they see movement. Pupil reaction – To light reaction (direct, consensual and swinging light test) and accommodation. In addition, ask the patient to frown, show their teeth and puff out their cheeks. Rub your fingers to create noise on one side and keep the other hand still, then switch hands. If hearing loss is identified, inspect the external auditory canals and the tympanic membranes. Then move the tuning fork neck to the patient’s ear canal so they can hear the sound. A normal response is that air conduction (ear) is better heard than bone conduction (mastoid). Weber’s test (lateralization) Apply tuning fork (256 Hz) to the top of patient’s head on middle of forehead. Turn the patient’s head against resistance, inspect and palpate the sternocleidomastoid muscle. Ask the patient to protrude their tongue – the tongue will deviate to the affected side. Best Eye Response Spontaneously 4 To speech 3 To pain 2 No response 1 Best Verbal Response Orientated 5 Confused 4 Inappropriate responses 3 Inappropriate sounds 2 No response 1 Best Motor Response Obeys commands 6 Localise to pain 5 Withdraws from pain 4 Flexion (decorticate) to pain 3 Extension (decerebrate) to pain 2 No response 1 Please record the patient’s Pupil size – 1–8 (mm), Pupil reaction – +: reacts, −: no reaction, c: closed eyes and Limb movement – Normal power, mild weakness, severe weakness, spastic flexion, extension and no response. Dysdiadochokinesia: Ask the patient to rapidly pronate and supinate their hand on the opposite hand, repeat in other hand. The patient may demonstrate variable distance between steps and difficulty with turning. As the patient’s finger approaches your finger a tremor may be noticed or there may be evidence of past-pointing. Staccato speech: Ask the patient to repeat ‘British constitution’ or ‘baby hippopotamus’. Ask the patient to heel-to-toe walk (as if on a tight-rope), walk on their toes and heals. Romberg test (to assess the dorsal columns of the spinal cord) – Ask the patient to stand with their feet together and ask the patient to close their eyes. Remember the anatomy of the spinal cord tracts: Descending pyramidal tract – Corticospinal tract (i. Specific Inspect the patient’s muscles for wasting, hypertrophy and involuntary movements (fasciculations, choreiform movements, tremor or jerks). Maintaining balance whilst standing relies on intact sensory pathways, sensorimotor integration centres and motor pathways. The first stage (standing with the eyes open) demonstrates that at least one of the sensory pathways is intact. Rapid alternating hand movements Ask the patient to simulate they are playing the piano. The patient should then tap the upward facing palm with their palmar and then doral aspect of their fingertips from the other hand. Lower limb function: Heal-shin test Ask the patient to raise one leg at the hip and place their heel of the flexed leg on their contralateral knee and then run their heel down the anterior surface of their shin towards their ankle. Heel-toe test of gait Ask the patient to walk in a straight line in order for the heel of one foot to be in contact with toes of their other foot. Examine the spinal segments with an anatomical system (follow the dermatomal distribution). The patient should also report the quality and quantity of this sensation (Figure 8. Upper limb Lower limb C5 Lateral arm L1 Below inguinal ligament C6 Thumb and index finger L2 Middle thigh C7 Middle finger L3 Lower thigh C8 Ring and small finger L4 Medial leg and medial foot T1 Medial arm L5 Lateral leg and dorsal foot S1 Lateral foot Pain function: Establish a baseline for sharpness (i. Examine the spinal segments with an anatomical system (follow the dermatomal distribution). Examine the spinal segments with an anatomical system (follow the dermatomal distribution). In the lower limbs, use the big toes, ankle (medial malleolus), tibial tuberosity or iliac crest. Two-point discrimination function: Assess discrimination by using an opened paperclip. If the reflex is absent, you may be able to enhance the reflex with reinforcement.
Cheap indinavir 400mg amex. Ms.