Stephens College. Q. Snorre, MD: "Order Dutasteride online no RX - Discount Dutasteride online OTC".
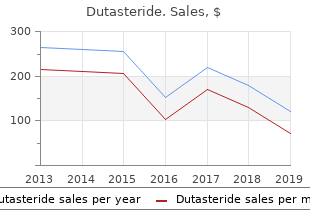
This should be reached after 3–4 months; in cases of very high baseline viral load it may take longer buy dutasteride 0.5 mg without a prescription revlon anti hair loss. However dutasteride 0.5mg on-line hair loss lyme disease, a viral load above the level of detection after six months of treatment almost always needs to be evaluated dutasteride 0.5mg sale hair loss in men 1920s. The same is true if a rebound in viral load is confirmed buy generic dutasteride 0.5mg on-line hair loss cure latest news. The more rapid and greater the decrease in viral load, the longer the therapeutic effect (Kempf 1998, Powderly 1999). In the early INCAS Trial, the relative risk of treatment failure in patients who had reached a viral load below 20 copies/ml was 20 times lower than in those who never reached 400 copies/ml (Raboud 1998). Virologic treatment failure can be recognized quite early. In practice, viral load should be monitored after four weeks on ART. This is useful not only to the patient for reasons of well-being (“less virus, more CD4 cells”). But it is also an important indi- cation for the continued success of treatment. If the viral load is not below 5,000 copies after four weeks of ART, later treatment failure is likely (Maggiolo 2000). If the viral load is not below 500 copies/ml or at least one log below baseline, the like- lihood of having a viral load of 500 copies/ml at week 24 is only 9% (Demeter 2001). In ACTG 5202, a less robust week 4 virologic response was associated with higher risk for subsequent virologic failure (Gant 2013). According to another prospective study, virological response can be predicted even after 7 days (Haubrich 2011). However, viral load testing after such short periods of ART in previously untreated patients is not clinical routine. Goals and principles of therapy 145 The cut-off point of 20 or 50 copies/ml is somewhat arbitrary. It is based on the currently available viral load assays. Whether 60 copies/ml are indeed worse than 30 copies/ml and indicate a lower success of treatment has yet to be proven. In the case of a persistent low level viremia (LLV) between 20 and 50 copies/ml, the risk of virological failure seems not to be increased (Charpentier 2012). There are, however, other studies suggesting an association between the level of viremia and virological failure, even at very low levels (Maggiolo 2012, Pugliuese 2013). Thus, the signifi- cance of LLV is still a matter of a debate. At such low levels, methodological inac- curacies must also be taken into account. A single detectable viral load “blip” to low levels (~1000 copies/ml) is often irrelevant (see below). Blips need to be distinguished from low, repetitive, measurable plasma viremia (50–400 copies/ml), in which the risk of resistance has been shown to be higher (Gunthard 1998, Nettles 2004, Taiwo 2012). If immune activation and inflammatory parameters are increased in these patients is still controversially discussed (Eastburn 2011, Taiwo 2012, Reus 2013). A viral load “below the level of detection” of 50 copies/ml means just that – no more, no less. A total of 50 copies/ml indicate that 5 liters of blood contain 250,000 virions; in addition, even more actively replicating viruses are present in the lymphatic organs. Thus, theoretically, a measurable viremia, even at very low levels, may possibly translate to a higher risk of resistance in the long-term. Perhaps there is indeed a relevant difference between 50 and 10 copies/ml with regard to the risk of developing resistance. Risk factors for virological failure are pre-treatment with antiretroviral agents (exist- ing resistance mutations) and low adherence. Whether the baseline CD4 T cell counts or the baseline plasma viremia play a role in treatment-naïve patients has not been conclusively proven (see chapter on When to Start ART). It seems that many other risk factors associated with virological failure or response are not known. A new area in this setting is pharmacogenetic research focusing on how genes influence an indi- vidual response to drugs. Investigators have begun to identify associations among human genetic variants, predisposition to HIV drug toxicities, and likelihood of viro- logic response. These include HLA typing and enzyme polymorphisms (Haas 2006). Pharmacogenomic testing will ultimately benefit persons living with HIV through better individualized treatment. More good news for today is that morbidity and mortality may be lowered signifi- cantly even if the viral load is not decreased to below the level of detection (Grabar 2000, Deeks 2002). Patients often remain immunologically stable for a long time, even with insufficient viral suppression. A large cohort study has shown that CD4 T cells do not drop as long as the viral load remains below 10,000 copies/ml or at least 1. However, with the new drug classes much more is possible now than in the 90s. Thus, plasma viremia should be reduced to below the detection limit in all patients. Little is known about how long treatments remain effective. The belief that treat- ment success is limited to only a few years is widespread. Many patients at the time were inadequately pretreated with mono- or dual-therapy, and had thus developed extensive resistance. In such patients, the effect of treatment was often limited, as even a single point mutation was often enough to topple a whole regimen. Today, especially in therapy-naïve patients without pre-existing mutations, the risk of treatment failure is much less. After almost 20 years of using combination ART, a very high number of patients still have viral loads below the level of detection. This is particularly true for patients who were adequately treated from the start (starting with triple therapy and/or rapid 146 ART switching of several drugs upon failure). One of the few trials with a longer follow- up period studied 336 antiretroviral-naïve patients who had reached a viral load below 50 copies/ml within 24 weeks (Phillips 2001). More detailed analy- sis showed that a large proportion of the patients experiencing viral rebound had actually interrupted ART. True virological failure was only seen in 14 patients, which corresponds to a risk of 5. Most importantly, the risk of virologi- cal failure decreased significantly with time.
Diseases
- Seckel syndrome 2
- Sclerosteosis
- Hypopituitarism
- Acquired immune deficiency syndrome
- Heavy metal poisoning
- Acute myeloblastic leukemia type 5
- Micro syndrome
- Liver neoplasms
- Renal dysplasia diffuse cystic
A Randomized Double-Blind Comparison of Coformulated Elvitegravir/Cobicistat/Emtricitabine/Tenofovir Disoproxil Fumarate Versus Efavirenz/Emtricitabine/Tenofovir Disoproxil Fumarate for Initial Treatment of HIV-1 Infection: Analysis of Week 96 Results dutasteride 0.5mg generic hair loss in men 1920. When to switch CHRISTIAN HOFFMANN Antiretroviral therapy has to be modified frequently order dutasteride 0.5mg free shipping hair loss and weight loss, even though the rates of mod- ification and interruptions have declined in recent years order 0.5mg dutasteride amex hair loss in men 1 disease. In EuroSIDA cheap dutasteride 0.5mg otc hair loss after bariatric surgery, among almost 1200 patients who began ART after 1999, at one year after initiation, only 70% of patients remained on their original regimen. In an evaluation of the Swiss Cohort, 42% of 1318 patients beginning ART between 2005 and 2008 had modified therapy after one year, 22% of them due to side effects (Elzi 2010). In general, ART is switched for three main reasons (interruptions will be discussed separately): • Acute side effects • Long-term toxicity (or concerns regarding them) • Virologic treatment failure 6. Switching due to acute side effects Not every acute side effect requires immediate modification. Mild nausea or diarrhea at the beginning can and should be tolerated. Gastrointestinal side effects that occur during the first weeks often improve spontaneously or can be treated symptomati- cally. The same is true for some allergic reactions and for mild CNS disorders. Talking with the patient, suggestions on how to tolerate or palliate certain problems with the idea that these will not continue indefinitely will help. However, certain adverse drug events almost always require discontinuation (see box). Side effects that almost always require discontinuation/change of ART • Severe diarrhea, which persists despite loperamide even after several weeks (usually with nelfinavir, lopinavir/r, fosamprenavir/r) • Severe nausea, which persists despite metoclopramide, which requires continu- ous treatment or leads to significant weight loss (usually AZT, ddI) • Persistent sleeping disorder (efavirenz) • Polyneuropathy (d4T, ddI, possibly also 3TC), often resolves very slowly • Severe anaemia (AZT) • Severe, progressive muscular weakness (d4T, ddI) • Pancreatitis (ddI, ddI+TDF, d4T+ddI, in rare cases lopinavir/r) • Lactic acidosis (most often d4T+ddI, but also all other NRTIs) • Severe allergies with involvement of mucous membranes, fever (typically aba- cavir, all NNRTIs, more rarely fosamprenavir or darunavir) • QT prolongation (saquinavir, but also other ARVs) • Renal failure (tenofovir/STRs, indinavir), nephrolithiasis (indinavir) • Hepatotoxicity with transaminases >5 x normal values (nevirapine, tipranavir) • Jaundice (nevirapine, atazanavir, indinavir, tipranavir) • Rhabdomyolysis (raltegravir) • Severe repetitive onychitis (indinavir, possibly also 3TC) • Depression, psychosis (efavirenz, possibly also AZT) 6. Switching due to concerns over long-term toxicity In the last few years, many clinicians have started to change virologically successful combinations out of concern for cumulative long-term toxicities, especially in cases of lipodystrophy and dyslipidemia. The switch strategy is based on the assumption that not all antiretroviral agents have similar toxicities. The most important switch studies are discussed below. PI replacement with other agents PIs may cause side effects in the long-term. Among these are lipodystrophy with abdominal fat accumulation and at the back of the neck, but also gastrointestinal side effects and dyslipidemia. Many randomized studies replacing a successful PI- based regimen by other drugs have been performed during recent years (Table 7. Taken together, these studies show that lipid levels are most likely to improve after switching to other agents, in particular rilpivirine, nevirapine and integrase inhibitors, and to a lesser extent, if ever, efavirenz. Quality of life and treatment sat- isfaction improved significantly in the switch arms of most studies, probably due to the reduced pill burden. In cases of lipodystrophy the effects are clearly poorer and less-well characterized. L better, LD better Becker 2001 EFV 346 Advantage L unchanged Molina 2005 EFV 355 Advantage L/LD n. L only better with NVP better, LD unchanged Calza 2005 EFV/NVP 130 n. L even worse (if PI-patients received statins) Palella 2014 RPV 476 n. L better PI → Triple Nuke Clumeck 2001 211 Advantage L better, LD subjectively better Opravil 2002 163 Disadvantage L better, LD unchanged (Trend) Katlama 2003 209* n. L better, LD better PI → NNRTIs or Triple Nuke Martinez 2003 EFV/NVP/ 460 Trend against L only better with ABC, ABC ABC LD unchanged PI → INSTIs Eron 2010 RAL 350 Disadvantage L better Martinez 2010+2012 RAL 139 n. L (and some biomarkers) better Arribas 2014 EVG/c 433 Advantage AEs similar In all studies (except Martinez 2003), randomization was against continuing PIs. All patients were on PIs for several months at the time of the switch, with unde- tectable viral load. VL=viral load in the switch arm versus the continuing arm. One example of what could happen when the drug is changed for strategic reasons is shown in Table 7. This case demonstrates how careful one must be when switch- ing drugs, if there is a past history of inadequate treatment (i. Since 1998 AZT+3TC+NFV (always under the limit of detection) n. Rash with hepatic involvement occurred on NVP, so in July 2003 NVP was replaced by 3TC – a triple nuke. The resistance mutations then detected were acquired almost certainly from the earlier treatment with AZT+ddC, but sufficiently suppressed while on PI therapy There is a risk of a higher failure rate when switching from PI based regimens to triple nuke, especially in patients with prior NRTI pretreatment (Bommenell 2011). A higher failure rate was also seen in the SWITCHMRK trials in patients switching to the integrase inhibitor raltegravir (Eron 2010). In these two large-scale Phase II studies, a total of 702 patients on a stable and functioning lopinavir-containing regimen were randomized to change to ralte- gravir or to continue with lopinavir. Lipids improved with the switch, but after 24 weeks a non-inferiority of raltegravir compared to lopinavir/r in efficacy was not seen. In the ITT analysis, only 82% of patients on raltegravir compared to 88% on the continued PI maintained viral load below the limit of detection after 24 weeks. The viral load breakthrough applied especially for pre-treated patients with previous therapy failure. A smaller open-label randomized study in Spain did not make the same observations, however. Patients had been below detection for a longer period (Martinez 2010). In STRATEGY-PI, a trial in which patients were randomized to the INSTI elvitegravir/c or to remain on their PI regimen, no rebounds were seen. However, in this study patients with complex pre-treatment were excluded, in order to avoid sobering results like SWITCHMRK, (Arribas 2014). With elvitegravir/c, less diarrhea but more nausea was observed. It is thus important to consider potential side effects of new agents when a switch from a PI is planned. Efavirenz may be associated with adverse CNS events. There is the risk of a hypersensitivity reac- tion with abacavir if HLA typing is not available. Of note, there is still no data on a change or a PI substitution with maraviroc or dolutegravir yet. Possibly the PI does not always have to be replaced with another drug class. In cases of dyslipidemia with lopinavir or fosamprenavir, switching to atazanavir could make sense as it is associated with a comparably good lipid profile (Gatell 2007, Soriano 2008, Mallolas 2009).
Diseases
- Sacral defect anterior sacral meningocele
- Hemoglobin C disease
- Cerebellar hypoplasia endosteal sclerosis
- Myasthenia gravis
- Omphalomesenteric cyst
- Polyposis, hamartomatous intestinal
The effects of losartan compared to atenolol on stroke in patients with isolated systolic hypertension and left ventricular hypertrophy cheap dutasteride 0.5 mg fast delivery hair loss postpartum. Klein G order dutasteride 0.5 mg visa hair loss treatment for men, Pfafferott C buy dutasteride 0.5 mg line hair loss using wen, Beil S buy dutasteride 0.5 mg on line hair loss radiation, Gehring J, Niemela M, Kendall MJ. Effect of metoprolol and amlodipine on myocardial total ischaemic burden in patients with stable angina pectoris. Efficacy and tolerability of 50 mg controlled release metoprolol (CR/Zok) once daily in comparison with conventional metoprolol 50 mg twice daily. Efficacy of monotherapy compared with combined antianginal drugs in the treatment of chronic stable angina pectoris: A meta-analysis. Hemodynamic effects at rest and during exercise of combined alpha/beta-receptor blockade and of beta-receptor blockade alone in patients with ischemic heart disease. Hemodynamic and adrenergic effects of combined alpha/beta- receptor blockade versus combined beta-receptor and slow channel calcium blockade in patients with ischemic heart disease. Sotalol vs metoprolol for ventricular rate control in patients with chronic atrial fibrillation who have undergone digitalization: A single-blinded crossover study. Kontopoulos AG, Athyros VG, Papageorgiou AA, Papadopoulos GV, Avramidis MJ, Boudoulas H. Effect of quinapril or metoprolol on heart rate variability in post- myocardial infarction patients. Korula J, Groszmann RJ, Lerner E, Bosch J, Garcia-Tsao G, Grace ND. Hemodynamic events in a prospective randomized trial of propranolol versus placebo in the prevention of a first variceal hemorrhage (2). Beta blockers Page 108 of 122 Final Report Update 4 Drug Effectiveness Review Project 240. Comparison of the duration of action of atenolol and nadolol for treatment of angina pectoris. Prevention of heart failure by antihypertensive drug treatment in older persons with isolated systolic hypertension. Kostis JB, Rosen RC, Brondolo E, Taska L, Smith DE, Wilson AC. Superiority of nonpharmacologic therapy compared to propranolol and placebo in men with mild hypertension: a randomized, prospective trial. Randomized comparison of antiarrhythmic drug therapy with implantable defibrillators in patients resuscitated from cardiac arrest : the Cardiac Arrest Study Hamburg (CASH). Essential hypertension of Caribbean hispanics: Sodium, renin, and response to therapy. Comparison of a fixed combination of nifedipine slow release and atenolol (BAY-R-1999) and nifedipine slow release alone in patients with stable angina pectoris: A multicenter, randomized, double-blind, parallel- group study. Current Therapeutic Research, Clinical & Experimental. Lai C, Onnis E, Pirisi R, Orani E, Delogu G, Cherchi A. Anti-ischaemic and anti-anginal activity of atenolol, nifedipine and their combination in stable, chronic effort angina. Lakshman MR, Reda DJ, Materson BJ, Cushman WC, Freis ED. Diuretics and beta- blockers do not have adverse effects at 1 year on plasma lipid and lipoprotein profiles in men with hypertension. Department of Veterans Affairs Cooperative Study Group on Antihypertensive Agents. Lamb RK, Prabhakar G, Thorpe JA, Smith S, Norton R, Dyde JA. The use of atenolol in the prevention of supraventricular arrhythmias following coronary artery surgery. Quality of life in the African American Study of Kidney Disease and Hypertension: effects of blood pressure management. American journal of kidney diseases : the official journal of the National Kidney Foundation. Nadolol for prophylaxis of gastrointestinal bleeding in patients with cirrhosis. Noradrenergic activity and silent ischaemia in hypertensive patients with stable angina: effect of metoprolol. Antihypertensive effect of the fixed combination nifedipine sustained release 20 mg + atenolol 50 mg in partial responders to calcium channel blockers: Parthenon pilot study. Current Therapeutic Research, Clinical & Experimental. Evaluating quality of life in hypertensive patients. Beta blockers Page 109 of 122 Final Report Update 4 Drug Effectiveness Review Project 256. Elective response to propranolol or verapamil in ischemia on effort. Effects of antihypertensive medications on vitality and well-being. Effects of atenolol, verapamil, and xamoterol on heart rate and exercise tolerance in digitalised patients with chronic atrial fibrillation. Cardiovascular morbidity and mortality in patients with diabetes in the Losartan Intervention For Endpoint reduction in hypertension study (LIFE): a randomised trial against atenolol. Efficacy and safety of bisoprolol and atenolol in patients with mild to moderate hypertension: a double-blind, parallel group international multicentre study. Angiographic evolution of coronary atherosclerosis in patients receiving propranolol. Nitrendipine and atenolol in essential hypertension in young and middle-aged patients: effect on serum lipids and left ventricular mass. Metoprolol versus clonidine in the prophylactic treatment of migraine. Coadministration of tamsulosin and three antihypertensive agents in patients with benign prostatic hyperplasia: pharmacodynamic effect. Lucio Ede A, Flores A, Blacher C, Leaes PE, Lucchese FA, Ribeiro JP. Effectiveness of metoprolol in preventing atrial fibrillation and flutter in the postoperative period of coronary artery bypass graft surgery. A comparative trial with flunarizine and propranolol in migraine. Lundell L, Leth R, Lind T, Lonroth H, Sjovall M, Olbe L. Evaluation of propranolol for prevention of recurrent bleeding from esophageal varices between sclerotherapy sessions.