Westminster Theological Seminary. T. Roland, MD: "Order online Meclizine cheap no RX - Proven Meclizine online".
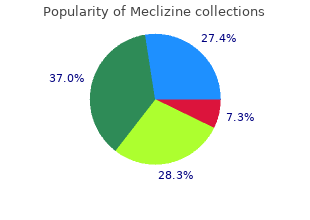
It is used extensively as an oxidizing agent in organic synthesis buy meclizine 25 mg free shipping medications nursing, for example buy meclizine 25 mg mastercard treatment 5cm ovarian cyst, for the oxidation of allylic alcohols order meclizine 25mg amex medications reactions. Nephelometric refers to the way the instrument cheap meclizine 25 mg visa medicine interactions, a nephelometer, measures how much light is scattered by suspended particles in the water. For substances it is usually expressed in parts per million (ppm), or sometimes in milligrams per cubic meter (mg/m ). The carbon in the biological treatment process acts as a "buffer" against the effects of toxic organics in the wastewater. If the level controller may be set with too close a tolerance 45 could be the cause of a control system that is frequently turning a pump on and off. These systems do not have to test or treat their water for contaminants which pose long-term health risks because fewer than 25 people drink the water over a long period. This agency sets federal regulations which all state and local agencies must enforce. The term often is used in a legal or regulatory context and in such cases the precise definition is a matter of law. The term may refer both to well characterized organic compounds and to mixtures of variable composition. This rule also applies to any system that mixes surface and groundwater if the groundwater is added directly to the distribution system and provided to consumers without treatment. Additional protection of groundwater from both chemical and microbial contamination from shallow wells (including cesspools) is expected to be provided as a result of recent revisions to the Underground Injection Control Regulations, published December 7, 1999 (19). Waterborne Diseases ©6/1/2018 269 (866) 557-1746 Surface water systems are also required to monitor for the presence of Cryptosporidium, Giardia, total culturable viruses, and total* and fecal coliforms or Escherichia coli >1 time/month for 18 months. Recreational Water Regulation of recreational water is determined by state and local governments. Standards for operating, disinfecting, and filtering public swimming and wading pools are regulated by state and local health departments and, as a result, are varied. The guideline recommends that the monthly geometric mean concentration of organisms in freshwater should be <33/100 mL for enterococci or <126/100 mL for Es. States have latitude regarding their guidelines or regulations and can post warning signs to alert potential bathers until water quality improves. Unlike treated venues where disinfection can be used to address problems with microbiological quality of the water, contaminated freshwater can require weeks or months to improve or return to normal. Prompt identification of potential sources of contamination and remedial action is necessary to return bathing water to an appropriate quality for recreational use. The intent of Beach Watch is to assist† state, tribal, and local authorities in strengthening and extending programs that specifically protect users of recreational waters. Data regarding water systems and deficiencies implicated in these outbreaks are used to assess whether regulations for water treatment and monitoring of water quality are adequate to protect the public against disease. Surveillance also enables identifying etiologic agents and environmental or behavioral risk factors that are responsible for these outbreaks. This information is used to inform public health and regulatory agencies, water utilities, pool operators, and other stakeholders of new or reemerging trends that might necessitate different interventions and changes in policies and resource allotment. The form solicits data related to 1) characteristics of the outbreak, including person, place, time, and location of the outbreak; 2) results from epidemiological studies conducted; 3) specimen and water sample testing; and 4) factors contributing to the outbreak, including environmental factors, water distribution, and disinfection concerns. Numerical and text data are abstracted from the outbreak form and supporting documents and are entered into a database before analysis. First, >2 persons must have experienced a similar illness after either ingestion of drinking water or exposure to water encountered in recreational or occupational settings. This criterion is waived for single cases of laboratory-confirmed primary amebic meningoencephalitis and for single cases of chemical poisoning if water-quality data indicate contamination by the chemical. Second, epidemiologic evidence (Table 1) must implicate water as the probable source of the illness. For drinking water, reported outbreaks caused by contaminated water or ice at the point of use (e. If both actual and estimated case counts are included on the outbreak report form, the estimated case count can be used if the population was sampled randomly or the estimated count was calculated by applying the attack rate to a standardized population. Of the approximately 170,000 public water systems in the United States, 113,000 (66. Community water systems serve approximately 264 million persons in the United States (96. These statistics exclude outbreaks associated with these sources because they are not intended for drinking and are not considered to be public water systems. Waterborne Diseases ©6/1/2018 271 (866) 557-1746 Also excluded from these statistics are the millions of persons who use noncommunity systems while traveling or working. In this surveillance system, outbreaks associated with water not intended for drinking (e. If >1 deficiency is noted on the outbreak report form, the deficiency that most likely caused the outbreak is noted. Deficiency classifications are as follows: 1: untreated surface water; 2: untreated groundwater; 3: treatment deficiency (e. Recreational waters include swimming pools, wading pools, whirlpools, hot tubs, spas, water parks, interactive fountains, and fresh and marine surface waters. Although outbreaks without water-quality data might be included in this summary, reports that lack epidemiologic data were excluded. Outbreaks of dermatitis and single cases of either primary amebic meningoencephalitis or illness resulting from chemical poisoning were not classified according to this scheme. Weighting of epidemiologic data does not preclude the relative importance of both types of data. The purpose of the outbreak system is not only to implicate water as the vehicle for the outbreak, but also to understand the circumstances that led to the outbreak. A classification of I indicates that adequate epidemiologic and water-quality data were reported (Table 1); however, the classification does not necessarily imply whether an investigation was optimally conducted. Outbreaks and the resulting investigations occur under various circumstances, and not all outbreaks can or should be rigorously investigated. Waterborne Diseases ©6/1/2018 272 (866) 557-1746 Results All related tables and figures are in the rear of this section Outbreaks Associated with Drinking Water During 1999--2000, a total of 39 outbreaks associated with drinking water were reported by 25 states (see Appendix A for selected case descriptions). One of the 39 outbreaks was a multistate outbreak of Salmonella Bareilly that included cases from 10 states. Of the 39 total drinking water outbreaks, 15 outbreaks were reported for 1999 and 24 for 2000. These 39 outbreaks caused illness among an estimated 2,068 persons; 122 persons were hospitalized, and two died. One of two outbreaks associated with a chemical etiology was not assigned a class because that outbreak was a single case of illness resulting from nitrate poisoning associated with consumption of water from a private well.
Where suspicion still exists cheap meclizine 25mg with mastercard when administering medications 001mg is equal to, vancomycin susceptibility may settle the question; all Gram positives except Lactobacillus discount 25mg meclizine medicine wheel teachings, Leuconostoc generic meclizine 25 mg on-line symptoms norovirus, Pediococcus and rare strains of Enterococcus are sensitive order meclizine 25 mg mastercard symptoms you are pregnant, while Acinetobacter and Moraxella are the only Gram negatives which may show sensitivity. Nalidixic acid and polymyxin susceptibility also correlate very well (though not perfectly) with ‘true’ Gram stain reaction—Gram positives are resistant, and Gram negatives susceptible, to both. Again, an oxidase negative and/or large-celled Gram negative bacillus which is penicillin susceptible should be viewed with suspicion unless it has been identified as belonging to a species which includes penicillin susceptible strains. Slow-growing Gram positive bacilli of fine morphology should be subjected to a modified Ziehl-Neelsen stain. The actual morphology of an organism is frequently characteristic and can sometimes be virtually diagnostic. The appearance of cells grown in the presence of a -lactam to which they are susceptible (eg, from the zone edge around a penicillin disc) can often be useful in deciding this; cocci tend to enlarge and disrupt spherically, while rods are prone to elongate. Other important properties that can be almost instantly determined are the catalase and oxidase (Kovacs method using a platinum (never nichrome) loop to inoculate an 18-24 hours old colony from a non-selective and non-differential medium to freshly prepared 1% tetramethyl-p-phenyldiamine dihydrochloride (reacts with cytochrome c to form a blue coloured compound; positive reaction must occur in 10 seconds) is the most satisfactory method) reactions. The single most important biochemical characteristic is undoubtedly the O-F reaction. Whether an organism utilises glucose fermentatively, oxidatively or not at all is a highly correlative criterion. It is important to realise that nonfermentative organisms are strict aerobes and vice versa. Given just the above criteria, Cowan and Steele’s initial tables purport to group all the bacteria one is likely to encounter in a clinical microbiology into a number of groups which lead on to further tables eventually allowing a firm identification. This is because of the broad groupings, with lack of due notice given to important exceptions; the fact that absolute positive and negative values of characteristics are given at the 85% level, which gives a fairly high probability of encountering an exception; because descriptions of genera are sketchy and sometimes wrong in failing to note important exceptions, while descriptions of species are virtually nonexistent; such basic properties as colonial and cellular morphology are rarely mentioned. So, anyone using Cowan and Steel should check the identification carefully against a description in Balows or Bergey. The tables in Balows are more complete, frequently quote percentages, and are usually accompanied by clear descriptions of species. The problem with Balows is that it largely presupposes enough knowledge to be able to get to the right table. The three keys—’Nonenterobacteriaceae Fermentative Gram Negative Bacilli’, ‘Non-fermenting Gram Negative Bacilli’ and ‘Fastidious Gram Negative Bacilli’—require only urea, indole, nitrate and lactose as additional tests and are very useful but there are problems getting there: How do you know a fermentative Gram negative bacillus is non- Enterobacteriaceae? Why does ‘Fastidious Gram Negative Bacilli’ not include Haemophilus, Brucella, etc? Probably the best scheme for identification of nonfermenting and fastidious Gram negative bacilli is the Weaver- Hollis scheme. However, even here there are problems: misread any one of the three prime separating criteria (O-F, MacConkey, oxidase) and you’ll quickly be right off the track; many of the tests are not ones normally used in the laboratory; some organisms are far more quickly and definitively identified by alternative procedures; referral to fuller descriptions of organisms is still required. These limitations can arise because the necessary data are not in the data base, because the tests employed have insufficient discrimination for particular organisms, or because a test gives incorrect results. It is possible to use reactions obtained in these systems to ‘manually’ identify organisms. However, a great deal of caution must Diagnosis and Management of Infectious Diseases Page 417 Identification of Isolates be applied here since different results may well be obtained using different methods—something that must be borne in mind whatever method you are using. It is always wise to set up the standard extra tests (motility, nitrate, O-F glucose, MacConkey) on any oxidase positive organism; also, any organism which shows only a few reactions after overnight incubation should be reincubated for a further 24 hours and the extra tests set up. For organisms which do not grow on MacConkey or on the usual susceptibility test agars, the addition of a few drops of sterile serum to the saline will improve the test. If no red colouration appears, add a small amount of zinc dust; a red colouration indicates no reduction of nitrate, while no red colouration indicates reduction of nitrate to nitrogen gas. However, failure is usually due to a failure of generated codes to appear in the compendium, rather than of misidentification. Direct identification and susceptibility testing of a suspension of centrifuged organisms from positive blood cultures is possible in many cases (93% accuracy overall); however, it will not work with such organisms as pneumococci, Neisseria and Haemophilus and may give erroneous results for oxacillin sensitivity of Staphylococcus aureus, several antimicrobial agents with enterococci, and ampicillin and cephalosporins with Citrobacter, Enterobacter and Serratia.. On xylose lysine deoxycholate medium, Salmonella appears as distinct black colonies due to H S2 production, and on Salmonella-Shigella agar as clear colonies with some H S2 production. Test first for urease production [converts urea to ammonium carbonate, giving an alkaline reaction; spot test positive in 2 minutes, tube test in 2 hours or less]. A heavy suspension is made of the suspected Salmonella in formal saline from the nutrient agar plate. To drops of this suspension are added 1 drop of polyvalent A-G and/or polyvalent A-S (somatic O antigens), polyvalent H (flagellar antigen) and Vi (capsular antigen) respectively. If polyvalent A-G and/or A-S and polyvalent H are positive and Vi negative, the organism is a Salmonella other than Salmonella typhi and can be further identified by specific agglutinations. If the somatic O antigens are negative, the suspension should be boiled and the agglutinations repeated. If the Vi reaction is positive, boil the suspension for 15 minutes and repeat the agglutinations. Shigella does not ferment xylose and appears as red, sometimes crenated, colonies on xylose lysine deoxycholate agar, clear on Salmonella-Shigella agar. Colonies of Aeromonas hydrophila are large, rhizoid, non-xylose fermenting and oxidase positive. Plesiomonas shigelloides is non-xylose fermenting, oxidase positive, non-haemolytic on blood agar. Diagnosis and Management of Infectious Diseases Page 418 Identification of Isolates Campylobacter is a microaerophilic Gram negative bacillus which grows at 42C. On Skirow’s medium (blood agar with vancomycin, polymyxin B and trimethoprim), the colonial morphology ranges from small discrete colonies through to swarming colonies which may cover the entire surface of the plate in a uniform film and can be easily missed. Campylobacter is oxidase and catalase positive and appears in a Gram stain as Gram negative delicate ‘seagull-like’ rods. Rapid hippurate discs are used to differentiate between Campylobacter jejuni (positive) and other thermophilic Campylobacter species (negative). Vibrio grows on thiosulphate citrate bile sucrose agar after 24 hours as 2mm colonies (Vibrio cholerae (sucrose fermenter): 2-3 mm yellow; Vibrio parahaemolyticus (lactose fermenter): 3-5 mm green). Fecal isolates are oxidase positive but this cannot be tested from thiosulphate citrate bile sucrose agar as false negatives occur. Colonies of Clostridium difficile on blood agar + cycloserine + cefoxitin agar after 48 hours of anaerobic incubation at 37C are large, grey, irregular and have a distinctive putrid smell. The organisms can be presumptively identified with > 90% accuracy by a combination of colonial morphology, Gram stain and simple tests (eg. This necessitates the use of a fairly heavy inoculum (usually several colonies), which in turn means that it should be used only where one is reasonably certain of being able to obtain an inoculum consisting entirely of one organism (especially since no purity check will be available when the strip is read). Note particularly that Escherichia coli will give reactions of Shigella if insufficient reaction occurs. Always be suspicious of an identification (in any system) based only on a few characteristics.
Triage in the Emergency Department Triage includes focused physical examination appropriate to the organ system order 25mg meclizine amex medicine versed, referred to in the chief complaint order 25 mg meclizine amex medicine 6 year program. For example buy cheap meclizine 25 mg line medicine lyrics, patients who have complained of earache must have an examination of the ear buy 25mg meclizine amex medications dispensed in original container. Triage should be routine daily operation and all patients presenting to an Emergency Department should be triaged on arrival by a specifically trained and experienced registered nurse. Triage for India Although many systems exist, a simple 3-tier system is recommended. It is in practice in India since 1997 and has been found to be efficient and practical. Category I (obvious life-threatening emergency): The physician must examine the patient with zero delay. Case examples include cardiac arrest, continuous seizures, acute severe chest pain, haematemesis, sudden loss of consciousness, major trauma with hypotension, etc. Although some of these patients initially may appear to have not-so-serious chief complaints, about 25% of these patients have high-risk conditions. The patient needs full evaluation and treatment by a physician within 10 minutes of arrival, since there could be potential instability to the vital observations. Case examples include dyspnoea, high fever, acute abdominal pain, acute confusion, severe pain, serious extremity injuries, large lacerations, etc. Case examples include chronic, minor, or self-limiting disorders, medication refill, skin disorders, mild adult upper respiratory tract symptoms, mild sore throat, blood pressure check, etc. High respiratory rates are one of the most sensitive indicators of severely ill or injured patients. The person performing triage should not judge whether the person might be exaggerating his or her pain. Selection of the candidates for admission to the course will be made on merit, on all India basis in government hospitals 4. Medium of Teaching: English Staffing Full time teaching Faculty in the ratio of 1:6 Minimum faculty: Five faculty by name should be available for the course. Chief Co-ordinator: Emergency physician /Anesthesiologist/ Gen Surgeon/Gen Physician Coordinators : Orthopedics surgeon, Emergency physician/ Physician/ cardiologist etc Roles of All Faculty should be defined clearly. Course objectives: At the end of the course the student will be able to • Describe the concepts and principals of Emergency Medical Care • Perform basic and advanced life/limb saving skill in pre-hospital & hospital setting • Apply clinical knowledge and practical skills to real life scenarios. Budget: There should be budgetary provision for Audiovisual aids, stationary, Library, secretarial help, contingency expenses etc Physical facility 1. Library- permission to use institute library having current text books, internet, trauma journal, Emergency medicine journals etc. Semester System with 20% of total grade as per grading system in internal assessment 3. Assessment should be as grading and report, not marks with written detail report on all the objectives of examination. Knowledge :Assess the knowledge of basic concepts, theory, and principles of Emergency medical care 2. Comprehension; Candidate should be able to recall the knowledge and discuss as per patient requirement 3. Application : The candidate should be able to apply this knowledge to specific situations 4. Analysis: Candidate should be able to divide a problem into its component parts 5. Synthesis: Candidate should have the ability to combine theory and practical skills to solve complex situations 6. Evaluation : Candidate should be able to judge whether an action finally taken is good or bad for the ultimate outcome of the victim. Last but not the least, Does the candidate have positive attitude for care of emergency patient. Number of days/hours It is commonly assumed that these are 180 working days in a year including the days earmarked for admissions and examination. It is presumed that these will be minimum of 360 days for theory & practical teaching in 2 years & with 6 working hours a day, the total member of working hours in a year will be – (360 x 6 = 2160 hours) based on this a 2yrs course. Module Days x hours Total hours ------------------------------------------------------------------------ 1. Setting of ventilator • Cardiovascular: Acute Coronary Event, Chest pain, Shock of different etiology, Tachycardia, Bradycardia, Cardiac arrest 1. The Chief coordinating multidisciplinary services under critical and stressful circumstances is complex and requires the services of a senior consultant with sufficient years of clinical / administrative experience. The main responsibility of the medical officer is to ensure that all patients coming to the department are stabilised and adequately treated with minimum amount of waiting time. The number of medical officers appointed will depend on the patient load and design of the department. Emergency Physicians/ General physicians; Paediatricians, General surgeons, Orthopaedic surgeons, obstetricians, Anaesthetists: From the district hospital or visiting specialist arranged through firm contractual agreements. Nursing Matron: The Nursing matron is responsible for coordinating the various nursing activities. She prepares the duty roster and ensures that the appropriate nursing staff be posted to the various facilities of the department. They should have ongoing training in emergency procedures, investigations and patient stabilisation. Further, they should ensure the replacement of all appropriate drugs in the resuscitation cart as well as miscellaneous disposables. Nurses should ensure the working condition of monitors and other electronic equipment and notify malfunction. They are trained in the knowledge and skills to assist medical and nursing personnel in the Emergency Department. They are the leading cause for long-term absence from work (> 2 weeks) in many countries. Their direct and indirect cost is considerable and their management utilizes a significant part of the gross national product of many countries. For the middle aged and elderly, early detection and treatment of osteoporosis and management of rheumatic diseases at an early stage with available agents can significantly reduce the risk of fractures, deformities and associated morbidity and mortality. This in totality justifies the need for developing a program on a district model for Musculo- skeletal disorders in the country. Special provision for providing Calcium and Vitamin D to infants and women of both child bearing age and post menopause for both prophylactic and therapeutic purpose. Management information system for monitoring and evaluation through a structured data base mechanism for gathering information on availability of manpower, logistics, performance and other relevant information pertaining to the programme. Based on the response, necessity of services and willingness of the states/ medical colleges for implementing the program the medical colleges will be selected on priority. The phase-wise inclusion of medical colleges would be as shown below in the table: Medical 2012-13 2013-14 2014-15 2015-16 2016-17 Total Colleges 10 30 35 25 20 120 New 40 70 105 130 150 150* Cumulative th 150* medical colleges include 30 medical colleges that are targeted to be covered in 11 th Plan and 120 new medical colleges proposed to be covered in the 12 Plan. Amputee rehabilitation These institutions will impart training disability prevention, detection and early intervention for undergraduate and post-graduate medical students and other health professionals. General Objectives- 1) To build capacity in the Medical Colleges for providing comprehensive rehabilitation services and to train adequate manpower required at all levels of Health Care Delivery System.

Importance of the Underlying Disease and Type of Transplantation The type of organ transplanted purchase meclizine 25 mg with visa medications 5 songs, the degree of immunosuppression purchase 25 mg meclizine otc treatment 1st metatarsal fracture, the need for additional antirejection therapy discount 25mg meclizine with amex medicine cat herbs, and the occurrence of technical or surgical complications order meclizine 25 mg fast delivery medications not to be crushed, all impact on the incidence of infection posttransplant. In each type of transplantation, there are patients in which the risk of infection is greater. Incidence of infection is higher in thoracic transplantation pediatric population than that in adult (17). Thrombocytopenia of <50 Â 10 /L for three days is frequent after liver transplantation and as such was not found to be an important contributor to bleeding. If severely ill patients with end-stage liver disease are selected appropriately, liver transplant outcomes are similar to those observed among subjects who are less ill and are transplanted electively from home (20). Patients receiving alemtuzumab for the treatment of allograft rejection are more prone to suffer opportunistic infections (23,24). Infections such as insertion site sepsis, endocarditis, pneumonia, candidiasis, or sternal infection may complicate 38% of support courses. The use of extended donors does not seem to increase the risk of poor outcome (31). The time of appearance of infection after transplantation is an essential component of the evaluation of the etiology of infection. Early infections occurring in transplant patients within the first month after transplantation are generally similar to that in nontransplant patients who have undergone major surgery in the same body area. Reactivation of latent infections and early fungal and viral infections account for a smaller proportion of febrile episodes during this period. Finally, late infections (after 6 months) may be caused either by common community pathogens in healthy patients or by opportunistic microorganisms in patients with chronic rejection. Some of these may not be evident during the initial examination, which should be frequently repeated. If the patient is still intubated and the chest X ray does not reveal infiltrates, the possibility of tracheobronchitis or bacterial sinusitis should be considered. Herpetic stomatitis and infections transmitted with the allograft or present in the recipient may also appear at this time. Intermediate Period From the second to the sixth month, patients are susceptible to opportunistic pathogens that take advantage of the immunosuppressive therapy. In this period, we may expect infection with immunomodulatory viruses and with opportunistic pathogens (P. Some bacterial infections such as listeriosis may appear at this time as primary sepsis or meningitis. Aspergillosis may be encountered in patients with risk factors or massive exposure (39) and toxoplasmosis in seronegative recipients of a seropositive allograft (40). At this time, fever of unknown origin should be managed almost as in immunocompetent hosts. However, the aforementioned opportunistic infections may compli- cate this late period in patients with chronic viral infection such as hepatitis B or C, which may progress to end-stage organ dysfunction and/or cancer. Patients requiring chronic hemodialysis or with malignancy or late rejection are also susceptible to opportunistic infections (Cryptococcus neoformans, P. Previous infections or colonization, exposure to tuberculosis, contact with animals, raw food ingestion, gardening, prior antimicrobial therapy or prophylaxis, vaccines or immunosuppressors, and contact with contaminated environment or persons should be recorded (42,43). History of residence or travel to endemic areas of regional mycosis (44) or Strongyloides stercoralis may be essential to recognize these diseases (45). Exposure to ticks may be essential to diagnose entities such as human monocytic ehrlichiosis, which may be potentially lethal in immunosuppressed patients (46). Certain complications may increase the risk of bacterial and fungal infections in the early posttransplant period (Table 2). They include long operation (over 8 hours), blood transfusion in excess of 3 L, allograft dysfunction, pulmonary or neurological problems, diaphragmatic dysfunction, renal failure, hyperglycemia, poor nutritional state, and thrombocytopenia (18,47–50). Within the exploration of the thoracic area, the consultant should visualize the entry sites of all intravascular devices, even if they “have just been cleansed. Sepsis, without local signs, may be the initial sign of postsurgical mediastinitis. When the sternal wound remains closed, a positive epicardial pacer wire culture may be a clue to sternal osteomyelitis (55). Its presence requires rapid debridement and effective antimicrobial therapy and should prompt the exclusion of adjacent cavities or organ infection. If ascites is present, it should be immediately analyzed and properly cultured to exclude peritonitis. We recommend bedside inoculation in blood-culture bottles due to its higher yield of positive results. Tenderness, erythema, fluctuance, or increase in the allograft size may indicate the presence of a deep infection or rejection. Finally, skin and retinal examinations are “windows” at which the physician may look in and obtain quite useful information on the possible etiology of a previously unexplained febrile episode. We have analyzed the value of ocular lesions in the diagnosis and prognosis of patients with tuberculosis, bacteremia, and sepsis (59,60). Cutaneous or subcutaneous lesions are a valuable source of information and frequently allow a rapid diagnosis. Viral and fungal infections are the leading causes of skin lesions in this setting. The biopsy of nodules, subcutaneous lesions, or collections may lead to the immediate diagnosis of invasive mycoses and infections caused by Nocardia or mycobacteria, among others. In a recent study, complete agreement between pre- and postmortem diagnoses took place in only 58% of a total 149 patients. Two-thirds of all missed diagnoses were infectious and disagreement was particularly prominent in the transplant population (complete agreement 17% and major error in 61%) in comparison with trauma patients (complete agreement 86%) or cardiac surgery group (69%). Approximately 25% of febrile episodes do not present with an evident focal origin and do not permit a straight syndromic approach (63). Therefore, the patient’s antecedents, type of transplantation, and time after surgery are essential. We systematically recommend to our residents to go over the viral, bacterial, fungal, and parasitic etiologies that should be excluded. Pneumonias occur predominantly in the early postoperative period, especially in the patients who require prolonged ventilation or are colonized or infected before transplantation. The crude mortality of bacterial pneumonia in solid-organ trans- plantation has exceeded 40% in most series (65,66). The clinical presentation and the differential diagnosis are similar to those in other critical patients. The incidence of bacterial pneumonia is highest in recipients of heart-lung (22%) and liver transplants (17%), intermediate in recipients of heart transplants (5%), and lowest in renal transplant patients (1–2%) (67–69). The crude mortality of bacterial pneumonia in solid-organ transplantation has exceeded 40% in most series (66). Gram-negative pneumonia in the early posttransplant period is associated with significant mortality. In another study, opportunistic microorganisms caused 60% of the pneumonias, nosocomial pathogens 25%, and community-acquired bacteria and mycobacteria 15% (64). Gram-negative rods caused early pneumonias (median 9 days), and gram-negative cocci, fungi, Mycobacterium tuberculosis and Nocardia spp.