Athena University. T. Hassan, MD: "Order Skelaxin - Quality online Skelaxin no RX".
The tip shape cheap 400 mg skelaxin otc muscle relaxant 750 mg, position of the lower lateral cartilage effective 400mg skelaxin spasm, and thick- ness of the overlying skin determine the appearance of the tip skelaxin 400 mg discount quercetin muscle relaxant. Other factors contributing to nose appearance include the fibrous attachments and abutments to the anatomic structures buy 400 mg skelaxin muscle relaxant guardian pharmacy. The fibrous attachments hold the lower lateral cartilages to the upper lateral cartilages, pyriform aperture, and caudal septum and support and determine the position of the tip. The lower lateral cartilages resemble a tripod in the tip framework; the medial crura is the lower leg, and the lateral crural complex provides the two upper legs. Several techniques have been used to modify the tip cartilage to change tip projection, rotation, and support. Refinement of the nasal tip and tip projection requires various types of grafts and knowledge of the tip support mechanism. Grafts are usu- ally taken from the septal cartilage, conchal cartilage, or costal cartilage. The types of grafts used for mechanical support are the col- umellar strut, septal extension graft, and lateral crural strut graft. The types of graft used for contouring and enhancement of nasal tip projection include the shield graft, cap graft, and onlay tip graft. It is a combination procedure involving suturing and nasal tip pro- similar to a columellar strut except that it is more stable jection enhancement. The purpose of this graft is to enhance nasal tip support, tip stability, tip projection, and columellar shape. This graft is inserted in a downward direction to the nasal spine between the alar cartilages, taking care not to detach the intercrural fibrous connection. In addition to enhancing nasal tip support, the columellar strut graft ensures that the columella is straight and has good projection. Lack of caudal septal support is the common cause of a drooping nasal tip, in addition to inad- equate lower lateral cartilage. The graft is commonly placed protruding toward the caudal and dorsal direction and creates good support for the caudal septum and also contributes to tip support. The advantages of this graft are that it enables stabilization at the base of the nose, provides excellent support to the nasal tip, prevents postoperative loss of tip projection and tip drooping, and elongates the nose. The caudal septal extension graft can be associated postoper- atively with stiffness of the nasal tip and a change in the feel of the upper lip, and these side effects should be discussed preop- eratively with the patient. The lateral crural strut graft uses autogenous cartilage, which is sutured to the deep surface of the lateral crura, provid- ing support, preventing valvular collapse, and improving alar position. These grafts are a versatile tool as they also provide additional tip support, projection, and rotation, thus controlling the degree of caudal protrusion of the septum and nasal tip. Lateral crural struts are useful in the correction of boxy nasal tips, malpositioned lateral crura, alar rim retraction, alar rim collapse (collapse of the external nasal valve), and con- cave lateral crura. If the skin is thick, crura extending into the tip to produce dome definition points. The graft edge must be smoothly carved and appropriately fixed to blend in with the underlying cartilage. To produce a natural appearance, a columellar strut is first inserted to strengthen the tip support, and then the onlay graft is placed to increase tip projection and camouflage tip irregu- larities. This graft combines tip contouring with the strength of the columellar strut in a single stable unit. The graft is stabilized through placement in a tight pocket in the precrural space when using an endonasal approach, or by suturing to the crura when using an open approach. In tip surgery, various surgical techniques can be used to alter tip shape, projection, and rotation. Direct manipulation of the lower lateral cartilage is often required in addition to tip graft- 40. Direct manipulation consists of excision of the cephalic A cap graft is a small graft that is placed in the space between portion to reduce the lateral crus volume and for suturing the middle crus to slightly elevate and refine the infratip lobule the medial crura together, also known as the suturing techni- area. This approach is rarely per- formed in Asian patients when a range of other procedures is required in addition to resection of the cephalic portion. In the delivery approach, the skin from the cartilage is sepa- rated to create a flap that can be pulled out of the nostril to expose the superficial surface of the cartilage. The lower carti- lage exposure allows for more procedures to be undertaken compared with the nondelivery approach. Although the endonasal approach is difficult, I experience a great amount of improvement in tip projection using columel- lar strut, caudal septal extension graft and onlay, or shield graft. The columellar strut is fixated between the middle crura and supported by the intercrural fibrous connection. In addition to enhancing nasal tip support, the columellar strut graft ensures that the columella is straight and has good projection. The open approach provides excellent visualization of the entire lower cartilage, which assists in accurate diagnosis on the existing natural anatomic position and permits better plan- ing, and accurate ease of optimal graft placement and suturing. Bilateral marginal incisions The disadvantages are a longer operation time, risk of tip are made and are connected by a transcolumellar incision, and edema, transcolumellar scarring, and difficultly in creating the soft tissue is elevated exposing the tip cartilage and the dor- 10,18 pockets for graft stabilization. I prefer to use low V-shaped incision across the colum- ella, making it unnoticeable, which is preferred because Asian noses have a shorter columella and if columella lengthening is 40. The open approach is recommended in secondary rhino- Nasal tip surgery remains the most challenging and debated plasty, trauma cases, and cleft lip nose cases. The ideal nose shape can be achieved the open approach are greater control of the surgery and bleed- using a combination of suturing techniques and nasal tip grafts. An example of improve- ment of tip projection using columellar strut, septal extension graft, and cap graft through endonasal approach. Frequently used grafts in rhinoplasty: ical support or for contouring or enhancement of projection. Nasal tip surgery using a modified septal extension graft by que and nasal tip grafting to improve tip projection, rotation, means of extended marginal incision. Practical Septorhi- maximizes the chances of an accurate diagnosis, precise graft noplasty: An Asian Perspective. Septal extension grafts revisited: 6-year experience in con- trolling nasal tip projection and shape. The boxy nasal tip: classification and management Lippincott Williams & Wilkins; 1999 based on alar cartilage suturing techniques. Ballert The nasal skin envelope is of paramount importance in rhino- and thickening the nasal skin to camouflage the underlying car- plasty. Preoperative planning begins with a thorough evaluation of the Thin skin has the tendency to contract and reveal underlying nose. As a result, great care must be taken in sculpting the car- freckled appearance and its inability to hide the nuances of the tilaginous framework to withstand the contractile forces while underlying cartilaginous framework. In addi- often identified by the presence of sebaceous glands, oily tex- tion to perfecting the underlying cartilaginous framework, the ture, and amorphous nasal appearance. This Palpation of the skin and its thickness in relation to the chapter will focus on techniques to improve results in the thin- underlying cartilaginous framework will aid in determining skinned nose by optimizing cartilage structure, avoiding pitfalls, the relative thickness of the skin and underlying subcutaneous Fig. Strong, thick nasal tip cartilages will compound the com- plexity of rhinoplasty in the thin-skinned patient.
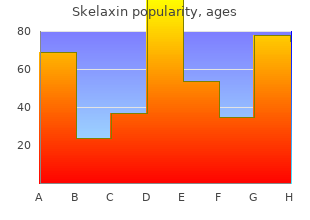
Lead screening is done cheap skelaxin 400mg with visa muscle relaxant overdose treatment, especially in high-risk areas cheap 400 mg skelaxin amex muscle relaxant valium, at 9 to 12 months of age and again at 2 years of age 400mg skelaxin visa spasms right arm. Cholesterol screening is performed in high-risk patients (those with positive family histories) older than 24 months generic 400 mg skelaxin mastercard muscle relaxant ointment. Sexually transmitted disease screening is performed yearly on all sexually active patients. Other specialized testing is accomplished depending on the child’s age, risk fac- tors, chief complaint, and conditions included in the differential diagnosis. Plain radiographs offer the advantage of inexpensive testing that reveals global views of the anatomy. Unfortunately, fine organ detail sometimes is not revealed which requires further radiographic study. Bone films for fracture, chest films for pneumonia, and abdomen films for ileus are common uses of this modality. Ultrasonography is a fairly inexpensive modality that requires little or no seda- tion and has no radiation risks. Because it is a slow procedure, sedation is often needed for younger children, and contrast is sometimes required. It allows for superb tissue contrast in mul- tiple planes, and excellent anatomic and functional imaging. It is frequently used to provide detail of the brain in patients with seizures or developmental delay, or to provide tissue detail on a mass located virtually anywhere in the body. It provides functional infor- mation (usually organ specific) but poor anatomic detail. Approach to Clinical Problem Solving There are generally four steps to the systematic solving of clinical problems: 1. The process includes knowing which pieces of information are more meaningful and which can be discarded. Experience and knowledge from reading help to guide the physician to key in on the most important concerns. A good clinician also knows how to ask the same question in several different ways and using different terminology, because patients at times will deny having been treated for asthma but will answer affirmatively to being hospitalized for wheezing. A diagnosis can be reached by systematically reviewing each possible cause and reading about each disease. Usually a long list of possible diagnoses can be pared down to two or three top suspicions, based on key labora- tory or imaging tests. For example, an adolescent presenting with a fever as the chief complaint can have an extensive differential diagnosis reduced to far fewer possibilities when the history reveals an uncle in the home with cough that con- tains blood, weight loss, and night sweats, and the physical examination shows an increased respiratory rate, lymphadenopathy, and right lower lobe lung crackles. Asthma categories range from mild intermittent (least severe) to severe persistent (most severe). For some conditions, such as syphilis, the staging depends on the length of time and follows along the natural history of the infection (ie, primary, secondary, or tertiary syphilis). If neither the prognosis nor the treatment was affected by the stage of the disease process, it would not make much sense to subcatego- rize something as mild or severe. As an example, mild intermittent asthma poses less danger than does severe persistent asthma (particularly if the patient has been intubated for asthma in the past). Accordingly, with mild intermittent asthma, the management would be intermittent short-acting β-agonist therapy while watching for any worsening of the disease into more serious categories (more severe disease). In contrast, a patient with severe persistent asthma would generally require short- acting β-agonist medications as well as long-acting β-agonists, inhaled steroids, and potentially oral steroids. Group A β-hemolytic streptococcal pharyngeal infection (“strep throat”) is associated with complications including poststreptococcal glomerulonephri- tis and rheumatic fever. The presence of group A β-hemolytic streptococcus confers an increased risk of problems, but neither the prognosis nor the treat- ment is affected by “more” group A β-hemolytic streptococcus or “less” group A β-hemolytic streptococcus. Hence, the student should approach new disease by learning the mechanism, clinical presentation, how it is staged, and how the treat- ment varies based on stage. Some responses are clinical, such as a change in the patient’s pain level or temperature, or results of pulmonary examination. The student must know what to do if the measured marker does not respond according to the expected. Is the next step to treat further, or to repeat the metastatic workup, or to follow up with another more specific test? Approach to Reading The student must approach reading differently than the classic “systematic” review of a particular disease entity. Patients rarely arrive to their health care provider with a clear diagnosis; hence, the student must become skilled in applying the text- book information to the clinical setting. Experience teaches that with reading; there are several crucial questions to consider thinking clinically. This is a difficult task to give to the medical student; however, it is the basic problem that will con- front clinicians for the rest of their careers. One way of attacking this problem is to develop standard “approaches” to common clinical problems. It is helpful to memorize the most common causes of various presentations, such as “the most common cause of mild respiratory distress in a term infant born by cesarean section is retained amniotic fluid (transient tachypnea of the newborn). The infant is term, large for gestation age, and was born by repeat cesarean section. Using the “most common cause” information, the student would guess transient tachypnea of the newborn. This question in many ways is even more difficult than the most likely diagnosis, because insufficient information may be available to make a diagnosis and the next step may be to pursue more diagnostic information. Another possibility is that the diagnosis is clear, but the subsequent step is the staging of the disease. Hence, from clinical data, a judgment needs to be ren- dered regarding how far along one is on the road of: Make diagnosis ã Stage disease ã Treatment based on the stage ã Follow response In particular, the student is accustomed to regurgitating the same information that someone has written about a particular disease but is not skilled at giving the next step. This talent is optimally learned at the bedside, in a supportive environ- ment, with freedom to take educated guesses, and with constructive feedback. The student in assessing a child in the hospital should go through the following think- ing process: 1. Based on the information I have, I believe that Cedric Johnson (a 3-month-old child with a positive respiratory syncytial virus nasal washing) has bronchiolitis. I don’t believe that this is severe disease (such as significant oxygen require- ment, severe retractions, or carbon dioxide retention on blood gas analysis). A chest radiograph shows no lobar consolidation (I believe this is important because a lobar consolidation would suggest a bacterial etiology). Therefore, the treatment is supportive care with supplemental oxygen and intravenous fluids as needed. I want to follow the treatment by assessing Cedric’s respiratory status (I will follow the oxygen saturation and degree of retractions), his temperature, and his ability to maintain his hydration orally without intravenous fluids. Also, if in the next few days Cedric does not get better or if he worsens, I think he will need a repeat chest radiograph to assess whether he has an evolving bacterial pneumonia. In a similar patient, when the clinical presentation is not so clear, perhaps the best “next step” may be diagnostic in nature such as blood cultures to determine if bacteremia is present.
Rapid clinical assessment is critical in case this patient is headed toward respiratory failure purchase skelaxin 400 mg otc spasms on left side of body, perhaps necessitating endotracheal intubation and mechanical vent ilat ion skelaxin 400 mg without a prescription vascular spasms. D uring an acut e 2 exacerbat ion order 400 mg skelaxin visa infantile spasms 2012, more severe hypoxemia or hypercapnia buy skelaxin 400 mg low cost spasms knee, or respirat ory acidosis not ed test to diagnose pulmonary diseases (Figure 15– 1). Spirometric tracings of forced the type of lung disease (obstructive vs restrictive), as well as potential revers- l ibility of airflow obstruction. Specific paramet ers h elp t o 1 1 classify the t ype an d degree of lun g dysfun ct ion ( Table 15– 1). Br on ch od ilat or s ( b et a-agon ist an d an t ich olin er gic agen t s) are ad m in ist er ed via handheld nebulizers; systemic glucocorticoids accelerate the rate of improvement in lung funct ion among t hese pat ient s; ant ibiot ics should be given if t here is suspi- cion of a respirat or y infect ion. Cont rolled oxygen administ rat ion wit h nasal oxygen at low flows or oxygen with Venturi masks will correct hypoxemia without causing severe hypercapnia. Caution must be exercised in patients with chronic respiratory insufficiency whose respiratory drive is dependent on “relative hypoxemia”; these individuals may become apneic if excessive oxygen is administered! Acut e 2 respiratory failure is generally treated with endotracheal intubation and mechani- cal vent ilat or y suppor t t o cor r ect the gas-exch an ge disor der s. Complicat ion s of mechanical ventilat ion include difficult y in extubation, ventilator-associated pneu- monia, pneumothorax, and acute respiratory distress syndrome. Pat ient s wit h a rest ing hypoxemia (PaO < 5 5 m m H g or S aO < 8 8 %) gen er ally b en efit from h om e oxygen 2 2 therapy, which must be utilized at least 18 h/ d. She complain s of fat igu e an d dyspn ea wit h m in imal exer t ion, an d a cou gh that is productive each morning. Inspirat ory st ridor would occur wit h upper airway, usually ext rat horacic, obst ruct ion. For patients with chronic hypoxemia, supplemental oxygen has a sig- nificant impact on mortality, with a greater benefit with continuous usage, rather than intermittent or nocturnal-only usage. Th e cough began ap p roximately 3 months p rior to this app ointment, and it has become more annoying to the patient. He has had a sedentary lifestyle but recently started an exercise program, including jogging, and says he is having a much harder time with the exertion. His examination is notable for a blood pressure of 134/78 mm Hg and lung findings of occasional expiratory wheezes on forced expiration. H e is n ormot en sive, an d h is respira- tory examination reveals an occasional expiratory wheeze on forced expiration. Confirmation of diagnosis: Spiromet r y wit h t est ing for bronch odilat or respon- siveness and bronchoprovocat ion test ing if indicat ed. Co n s i d e r a t i o n s This is a 37-year-old man who presents with a chronic cough of more than 8 weeks’ duration. W ith the history of exercise intolerance, worsening cough at night, and occasional wheezes on examinat ion, asthma is the most likely diagnosis in this patient. A chest radiograph is important to evaluate for more serious processes such as t umor, infect ion, or ot h er et iologies of lung injury. Bacterial infections causing subacut e cough are usually due t o pert ussis, Chlamydia, or mycoplasma. P h ysiologically, cou gh is a r eflexive d efen se mech an ism t o clear the upper airways. The action of cough serves two main functions: (1) to protect the lungs against aspiration and (2) to clear secretions or other material into more proximal airways to be expectorated from the tracheobronchial tree. Evaluation begins with a detailed history and physical examination, including smoking habits, complet e m edicat ion list, envir on ment al an d occupat ion al exp osu r es, an d any h is- tory of lung disease. Specific questions regarding the precipitating factors, duration and nature of t he cough should be elicited. Although t he physical examinat ion or nature of the cough rarely identifies the cause, meticulous review of the ears, nose, throat, and lungs may suggest a particular diagnosis. End- expiratory wheezing suggests active bronchospasm, whereas localized wheezing may be consistent with a foreign body or a bronchogenic tumor. Ch ron ic cough in an immun ocompr omised pat ient is beyon d the scope of this discussion. O ften, a definitive diagnosis for chronic cough depends on observing a successful response to therapy. Referral to a pulmonologist is recommended when the diagnostic and empiric therapy options are exhausted. Managing cough as a defense mechanism and as a symptom: Aconsensus panel report of the American College of Chest Physicians. Init ial t reat ment for a nonallergic et iology usually includes combinat ion t reat - ment with a first-generation antihistamine and a decongestant for 3 weeks. For allergic rhinit is, a newer-generat ion ant ihist amine, along wit h a nasal cort icost e- roid, should be used. Opacification, air-fluid levels, or mucosal thickening could suggest sinusit is, which should be t reat ed wit h ant ibiot ics. As t h m a Ast hma is a chronic inflammatory disease of the airways characterized by airway obstruction, bronchial hyperresponsiveness, and mucus hypersecretion with recur- ring symptoms, that is often reversible spontaneously or with treatment. Although wheezing is considered a classic sign of asthma, cough is often the only symptom. Cough-variant asthma usually presents with a dry cough that occurs throughout the day and night and is worsened by airway inflammation from viral infect ions of t he upper respiratory t ract, allergies, cold air, or exercise. Alt hough t he history may be suggestive of asthma, the diagnosis should be confirmed with pul- monary function tests. Approach t o ast h ma man agement 1 is stepwise wit h use of ast hma cont rollers such as inhaled cort icosteroids (and if needed systemic corticosteroids) which inhibit airway inflammation and broncho- dilators for rapid relief of symptoms. Current guidelines emphasize a preventative approach and a stepwise approach to t herapy based on ast hma severit y and cont rol (Table 16–1). Gastroesophageal Reflux Disease Gastroesophageal reflux disease often can be clinically inapparent, and it may be the primary or coexisting cause of the cough, as a result of aspiration and vagal st imulat ion. Init ial t reat ment includes lifest yle modificat ion along wit h medical therapy. Recommendations include a low-fat diet, elevation of the head of the bed, avoidance of offending foods (caffeine, alcohol, chocolate), smoking cessa- tion, and weight reduction. If acid suppression does not resolve the symptoms and if there are other symptoms of dyspepsia, a gastric motility stimulant such as metoclopramide may be considered. Patients who remain symptomatic after maximal medical treatment may benefit from 24-h ou r esoph ageal pH mon it or in g t o con fir m the d iagn osis. An esoph ago- gast r odu od en oscopy sh owin g esoph agit is or an u p p er gast r oint est in al r ad iogr aph ic series demonstrating reflux further supports the diagnosis. O f note, gast rointesti- nal symptoms may resolve prior to resolution of the cough, and full resolution may require 2 to 3 months of intensive medical therapy.
Order 400 mg skelaxin free shipping. Dental Tips For Healthy Teeth in Telugu | Dental Hygiene Tips | Telugu Updates.