Randolph College. K. Sulfock, MD: "Order Zebeta online no RX - Safe Zebeta no RX".
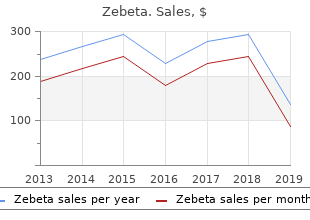
Typically appears as a large generic 10mg zebeta overnight delivery blood pressure chart height, hyperechoic order zebeta 5mg with visa arrhythmia that makes you cough, homogeneous mass zebeta 5mg low cost blood pressure taking, often containing shadowing calcification zebeta 5mg line blood pressure medication and cranberry juice. Undifferentiated (embryonal) Unusual hepatic malignancy found in children and young adults. The sonographic appearance ranges sarcoma from a multiseptate cystic mass to an inhomogeneous, predominantly echogenic solid lesion. Biliary cystadenoma/ Typically produces large, multicystic, septated mass that may have mural nodules. Sonogram shows mixed echogenicity and calcification (curved arrow) within a mass (straight arrow). Features suggestive of fatty infiltration include the lack of mass effect or dis- placement of hepatic vessels and the rapid change with time. Axial sonogram of the liver shows an ovoid, uniformly hyperechoic focus (arrow) consistent with a localized collection of fat. Axial sonogram shows uniformly hyperechoic a diffuse pattern of patchy hyperechoic foci (arrow) simulating lesions (arrow). Other underlying causes include obesity, diabetes, chemotherapy, parenteral nutrition, protein malnutrition, intestinal bypass operations, steroid therapy, inflammatory bowel disease, severe hepatitis, carbon tetrachloride toxicity, hyperlipidemia, and congestive heart failure. At times, fatty infiltration may involve only portions of the liver, producing discrete areas of increased echogenicity alternating with normal parenchyma (may be confused with metastatic disease). Cirrhosis should be suspected if the hepatic size is decreased and when there is nodularity of the liver surface, accentuation of fissures, coarsening of hepatic architecture, enlargement of the caudate lobe, regenerating nodules, ascites, or signs of portal hypertension. Careful sagittal scans of the left lobe should be performed to detect the recanalized umbilical vein, an indicator of portal hypertension. Sagittal scan demonstrates a diffuse in- 108 densely echogenic focus within the liver. In most normal patients, the liver and kidney parenchyma are very similar in their gray-scale texture (echogenicity of the liver may be slightly higher). A definite mismatch of the two tissues is strong evidence for parenchymal disease of the organ showing the greater echogenicity. Transverse scan shows a small, contracted liver liver secondary to chronic hepatitis. Transverse scan ity of the liver, with multiple hyperechoic lesions throughout the shows multiple venous collaterals (arrowheads). In chron- ic hepatitis, the parenchymal echo pattern is coarsened because of periportal fibrosis and inflammatory cells. Note the decrease in the brightness and number of the portal vein radicle walls (arrow). Note the increased brightness of the band through the mid-portion of the liver, corresponding to the maximum zone of sensitivity. The portal vein radicle walls seen within this bright zone have no internal echoes (arrows). Also may occur with hepatic metastases (mucinous tumors of the gastrointestinal tract in adults, neuroblastoma in children). If there is no history of previous surgery, the most common causes are gallstone ileus and penetrating duodenal ulcer disease. The calcified wall is sharply delin- eated and there is posterior acoustic shadowing. Sagittal sonogram of the right lobe of the liver shows a linear band of shadowing stones (arrows) in the bile ducts. The bile ducts are close to the edge of the liver, an appearance that reflects marked atrophy of the involved hepatic segment. Shadowing lesions due to portal vein gas appear in the periphery of the liver, unlike the more central location when the shadowing is secondary to gas in the biliary tree. Normal shadowing On sagittal scans near the neck of the gallbladder in normal patients, there is often a discrete shadow projected on the posterior aspect of the liver. This may be secondary to a refractive effect caused by tangential incidence of the ultrasound beam to the interface between the liver and gallbladder or to either thick fibrous tissue surrounding the right portal vein or the spiral valves of Heister in the gallbladder. Decubitus scans are required to search for tiny biliary calculi that may be lodged in the cystic duct and produce a similar appearance. Although more wall, no internal septations, and no contrast frequently single, hepatic cysts may be multiple enhancement. May occasionally be difficult to differentiate from a cystic neoplasm or an old hematoma (on ultrasound, cystic tumors may have internal septations and irregular inner margins, whereas non-neoplastic hepatic cysts have no internal septations and have completely smooth walls). May appear stage of a small tapeworm, for which dogs, sheep, multilocular with internal septations repre- cattle, and camels are the major intermediate senting the walls of daughter cysts. The wall of the cyst may show dense calcification, and gas may form in the cyst because of superimposed infection or communication with the intestinal lumen through the bile duct. The rare finding of a fat-fluid level in an echinococcal cyst has been reported as an indication of com- municating rupture into the biliary tree. After aspiration and the instillation of alcohol, there was virtual ablation of the cyst. The dilated cystic segments contain bile and communicate freely with the biliary tree and with each other, in contrast to polycystic liver disease in which the cysts contain a clear serous fluid and do not communicate with the biliary tree or other cysts. No enhancement after intravenous ductal system), hematogenous spread via the injection of contrast material, though a rim of portal venous system, generalized septicemia tissue around the cavity may become denser with involvement of the liver by way of the than normal liver (also seen with a necrotic hepatic arterial circulation, direct extension from neoplasm). May be solitary or multilocular (a single abscess is usually located in the right lobe). The demonstra- tion of gas in a low-density hepatic mass is highly suggestive of an abscess. No enhancement after intravenous are solitary, with the remainder being multiple and injection of contrast material, though a rim of often coalescing into a single large liver abscess. Well-circumscribed, fluid-attenuation of the liver that contains low-attenuation areas mass (consistent with a simple cyst) in the posterior portion reflecting early liquefaction. The abscesses are usually scattered rather uniformly throughout the liver, spleen, and even the kidneys. Although the liver filters out most of the resultant embryos, those that are not destroyed become hepatic hydatid cysts Echinococcus Multiple, irregular, ill-defined low-attenuation Rare alveolar form of Echinococcus infection, multilocularis lesions scattered through the liver. The appearance may mimic either metastases or pyogenic abscesses, though unlike these conditions in E. Other common findings are eventually leads to fibrosis and presinusoidal capsular calcification, junctional notches or hypertension. The eggs themselves do not survive depressions, an irregular hepatic contour, and and may subsequently calcify. Chronic infection extension of periportal vein deep into the results in cirrhosis and an increased risk of devel- liver resulting from fibrosis and parenchymal oping hepatocellular carcinoma. Numerous low-density lesions in a massively enlarged liver representing multiple abscesses containing Candida albicans.
They are usually due to chronic constipation but may also be the cause of constipation zebeta 5mg discount heart attack jack 1 life 2 live. Although they are usually considered to be a disease order 10 mg zebeta mastercard blood pressure medication makes me feel weird, it is important to remember that they may be a sign of cirrhosis of the liver and other conditions associated with portal hypertension 5mg zebeta visa blood pressure value ranges. As such buy 10mg zebeta amex pulse pressure how to calculate, they may point to the diagnosis of esophageal varices in cases of hematemesis, and their absence would make this diagnosis unlikely. Hepatomegaly with jaundice may make one think of hemolytic anemias; toxic or infectious hepatitis; bile duct obstruction due to stones, carcinoma of the pancreas, or ampulla of Vater; and biliary cirrhosis. Hepatomegaly with fever should make one think of viral hepatitis, infectious mononucleosis, ascending cholangitis, and other infectious diseases. Hepatomegaly and splenomegaly should make one think of alcoholic cirrhosis, amyloidosis, reticuloendotheliosis, various hemolytic anemias, biliary cirrhosis, and myeloid metaplasia. The presence of hepatomegaly with jaundice and enlarged gallbladder is characteristic of bile duct obstruction due to carcinoma of the pancreas, bile ducts, or ampulla of Vater. The clinician should remember that hydrops of the gallbladder with a common duct stone can mimic the same clinical presentation. Massive splenomegaly is characteristic of Gaucher’s disease, kala azar, and myeloid metaplasia. Occasionally, other forms of reticuloendotheliosis may also be associated with massive splenomegaly. Tenderness of the liver is seen with viral or toxic hepatitis, congestive heart failure, and ascending cholangitis. Metastatic neoplasms 315 and the various forms of cirrhosis may be diagnosed by liver biopsy, but one should keep in mind that it is dangerous to do a liver biopsy if biliary cirrhosis is suspected. Gallbladder ultrasound or cholecystography should be done if cholecystitis and cholelithiasis are suspected. Exploratory surgery may be the only way to get a diagnosis, especially in obstructive jaundice. The various infectious diseases will need antibody titers and skin tests to pin down the diagnosis. The various hemolytic anemias may be diagnosed by blood smears, a sickle cell preparation, serum haptoglobin, and hemoglobin electrophoresis. Hemochromatosis is also diagnosed by liver biopsy, but a test for serum iron and iron-binding capacity should also be done. Most physicians prefer to refer the patient with hepatomegaly to a gastroenterologist once the preliminary studies have been done. The presence of fever should make one think of pneumonia with pleurisy, pericarditis, subdiaphragmatic abscess, and peritonitis. The presence of heartburn and regurgitation should make one think of a hiatal hernia and esophagitis. Because they irritate the phrenic nerve, mediastinal masses such as Hodgkin’s disease, bronchogenic carcinoma, and esophageal carcinoma may cause hiccups. Hiccups may occur in tabes dorsalis, syringomyelia, encephalitis, chorea, and cerebral hemorrhage. If these are negative, it may be wise to evaluate the response to Pepto-Bismol or lidocaine viscous. If there is relief from one of these, the patient may well have a reflux esophagitis. If there is still confusion at this point, a gastroenterologist should be consulted before ordering other expensive diagnostic tests. Esophageal manometry and pH monitoring of the distal esophagus may also help in this regard. Following the algorithm, you do a neurologic examination and perform a straight leg raising test with negative results. She has a positive Patrick’s sign and exquisite tenderness over the greater trochanter. You diagnose greater trochanter bursitis and infiltrate the bursa with 1% lidocaine, which relieves her pain and restores her range of motion of the right hip. The presence of positive straight leg raising tests or other neurologic signs would suggest a herniated disk, a cauda equina tumor, or other neurologic disorders of the lumbar spine. Meralgia paresthetica will cause characteristic loss of sensation in the distribution of the lateral femoral cutaneous nerve. Is there a positive Patrick’s test or limitation of the range of motion of the hip? These findings suggest a greater trochanter bursitis or hip joint pathology such as fracture, osteoarthritis, rheumatoid arthritis, metastasis, slipped femoral epiphysis, Legg– Calvé–Perthes disease, rheumatic fever, or transient synovitis. Tenderness of the greater trochanter bursa will help differentiate greater trochanter bursitis. If the patient is a child, transient synovitis, slipped femoral epiphysis, Legg–Calvé–Perthes disease, and rheumatic fever should be considered. If the patient is an adult, it is more likely that the problem is osteoarthritis, a fracture, rheumatoid arthritis, metastasis, or avascular necrosis. A history of trauma would suggest that there is a fracture or a sprain of the hip joint, but the clinician should remember that a fracture in the elderly often occurs with no history of trauma. A trigger point injection of the greater trochanter bursa or ischiogluteal bursa will assist in the diagnosis of these conditions. These findings would suggest an ovarian tumor, an adrenal tumor or hyperplasia, chromosome mosaicism, and true hermaphroditism, which is rare. Adrenocortical steroids, testosterone, phenytoin, minoxidil, and diazoxide are just a few of the drugs that may cause hirsutism. The presence of an ovarian mass should make one think of polycystic ovaries, an arrhenoblastoma, or granulosis cell tumor. Remember, there may be no ovarian mass in polycystic ovary syndrome (Stein–Leventhal syndrome). An overnight dexamethasone suppression test is more accurate than a routine free cortisol in diagnosing Cushing’s syndrome. Intermittent hoarseness would suggest myasthenia gravis, urticaria, occupational causes, reflux esophagitis, tobacco, and alcoholism. If there are other abnormalities on the neurologic examination, one should consider peripheral neuropathy, poliomyelitis, Guillain–Barré syndrome, brain stem tumors, and cerebrovascular disease. Laryngoscopy will identify many intrinsic lesions of the vocal cords such as carcinoma, singer’s nodes, polyps, tuberculosis, or syphilis. It will also identify vocal cord paralysis due to carcinoma of the lung, aortic aneurysm, cardiac enlargement, or other mediastinal tumors. A normal laryngoscopic examination would suggest hysteria, myxedema, or acromegaly. Laryngoscopic examination is rarely necessary unless the acute hoarseness becomes chronic. The laryngoscopic examination is the single most important test for chronic hoarseness.
Syndromes
- Hematin given through a vein (intravenously)
- Large blood clot (hematoma)
- Other tetracycline antibiotics
- Brain or nervous system disorder
- Multiple sclerosis
- Long-term pain
The large loop is followed by the seromuscular layer of a bowel or gastric anastomosis is a small loop order 5 mg zebeta free shipping heart attack craig yopp, which catches only 4–5 mm of linea alba on each the Lembert stitch (Fig generic zebeta 5 mg overnight delivery blood pressure symptoms. The purpose of this small loop is to orient the abdominal 5 mm of tissue proven zebeta 5 mg blood pressure upper limits, including a bite of submucosa generic 10 mg zebeta overnight delivery blood pressure medication gluten free, and emerges wall in perfect apposition. Under proper Hemostatic Figure-of-Eight Stitch circumstances, it may be applied in a continuous fashion. The classic hemostatic figure-of-eight stitch is used for occlusion of a bleeding vessel that has retracted into the mus- Cushing Stitch cle or similar tissue. The Cushing stitch is similar to the Lembert stitch, except it is inserted parallel to and 2–4 mm from the cut edge of the Single-Layer Bowel Anastomosis bowel. It should catch about 5 mm of the bowel, including the Bowel anastomoses employing one layer of sutures have submucosa. An effective method for accomplishing approximation for anastomoses in poorly accessible loca- inversion and approximation simultaneously is the use of the tions, such as the low colorectal anastomosis. When used as a catches the seromuscular and submucosal layers and a small continuous stitch (Fig. When properly applied, it produces slight tive to the Connell stitch for inverting the anterior mucosal inversion of the mucosal layer and approximation. The main difference between the necessary to pass this stitch deeper than the submucosal layer. Connell stitch (see below) and a continuous Cushing suture is If it is passed into the lumen before emerging from the that the former penetrates the lumen of the bowel, whereas mucosal layer, it is identical with that described by Gambee, the latter passes only to the depth of the submucosal layer. Cushing stitch the danger that when tied with excessive 4 Dissecting and Suturing 33 a b Fig. The suture is placed loosely to avoid purse- stringing the anastomosis and hence is inadequate to produce hemostasis for small arterial bleeders. As the bowel is tension, it causes strangulation of a larger bite of tissue than inverted, intraluminal bleeding does not remain visible to the does the Lembert suture. This is particularly common with the stomach, which has a rich submucosal blood supply. Continuous Locked Stitch Rather than rely on the Connell stitch, individually ligate the Figure 4. When hemostasis is not a problem, some surgeons prefer to Technique of Successive Bisection close this layer with a simple over-and-over continuous stitch (see Fig. The technique we named “successive bisection” ensures consistently accurate intestinal anastomoses, especially Connell Stitch when the diameters of the two segments are not identical. The third is then inserted at a point that exactly bisects method for inverting the anterior mucosal layer of a two - the entire layer. It is obvious that the one-layer anastomosis does not turn in as much intestine and consequently has a larger lumen than the two-layer anastomosis. However, in the absence of postoperative leakage, obstruction at the anas- tomotic site is rare except perhaps when the esophagus is involved. It seems reasonable, though, to assume that if the seromuscular layer sutured by the surgeon suffers from some minor imperfection the mucosal sutures may compensate for the imperfection and prevent leakage. Although we have had good results with one-layer techniques, we recommend that each surgeon master the standard two-layer technique before considering the other. In most situations, the end-to-end technique is satisfactory for joining two segments of bowel. If there is some disparity in diameter, a Cheatle slit is performed on the antimesenteric border of the narrower segment of intestine to enable the two diameters to match each other (Figs. Chromic catgut is useful for approximating the mucosal There are two instances in which the end-to-side anastomo- layer during two-layer anastomosis of the bowel. Bear in mind that wound infec- reported that for the esophagogastric anastomosis following tion increases the rapidity of catgut digestion. Chromic cat- esophagogastrectomy, the incidence of leakage, postoperative gut has largely been supplanted by synthetic absorbable stenosis, and mortality is distinctly less with the end-to-side sutures for the purpose. This is probably true also for an esophagojejunal Chromic catgut swells slightly as it absorbs water after anastomosis. The second instance is the low colorectal anasto- contact with tissue, with the knots becoming more secure. With this procedure, the ampulla of the rectum is often is used for some endoscopic pretied suture ligatures for this much larger in diameter than the descending colon. Similarly, hydrated chromic catgut suture become soft and thus may be preferred for splenorrhaphy or hepatorrha- Sutured or Stapled Anastomosis? When are far superior to catgut because the rate at which they are done by surgeons whose techniques are sophisticated, sta- absorbed is much slower. About 20 % of the tensile strength pling and suturing can achieve equally good results. Consequently, the proteolytic enzymes in an area jejunostomy), whereas others are more rapidly and easily of infection have no effect on the rate of absorption of the stapled. Another, less obvious one, would be the stapled compared to that seen with catgut. However, these factors appear to be minor dis- advantages, and these products have made catgut an obsolete Suture Material suture material for many purposes. Absorbable Sutures Nonabsorbable Sutures Plain Catgut Plain catgut is not commonly used during modern surgery. Natural Nonabsorbable Sutures Although its rapidity of absorption might seem to be an advan- Natural nonabsorbable sutures, such as silk and cotton, have tage, this rapidity is the result of an intense inflammatory reac- enjoyed a long period of popularity among surgeons the tion that produces enzymes to digest the organic material. They have the advantage of easy handling and Plain catgut is acceptable for ligating bleeding points in the secure knot tying. Electrocautery the other hand, they produce more inflammatory reaction in has largely rendered that application unnecessary. Silk and cotton, Chromic Catgut although classified as nonabsorbable, disintegrate in the tis- Chromic catgut has the advantage of a smooth surface, which sues over a long period of time, whereas the synthetic mate- permits it to be drawn through delicate tissues with minimal rials appear to be truly nonabsorbable. It thus may be good for splenorrhaphy or hepator- disadvantages, silk and cotton have maintained worldwide rhaphy. Moisten the chromic catgut with saline and allow it popularity mainly because of their ease of handling and sur- to soften for a few seconds before inserting the suture. Because there are no Chromic catgut generally retains its strength for about a clear-cut data at this time demonstrating that anastomoses week and is suitable only when such rapid absorption is performed with synthetic suture material have fewer compli- desirable. It is completely contraindicated in the vicinity of cations than those performed with silk or cotton, it is not yet the pancreas, where proteolytic enzymes produce premature necessary for surgeons to abandon the natural nonabsorbable absorption, or for closure of abdominal incisions and hernia sutures if they can handle them with greater skill. Chassin With the exception of the monofilaments, a major disad- Prolene size 4-0 on atraumatic needles has been used for the vantage of nonabsorbable sutures is the formation of chronic seromuscular layer of intestinal anastomoses. This problem is and various braided polyester sutures have achieved great especially marked when material larger than size 3-0 is used popularity for vascular surgery. For this reason, many surgeons do not use nonabsorbable sutures Monofilament Stainless Steel Wire above the fascia.
When there is hypocalcaemia calcium gluconate will need to be added to the parenteral fluid generic 5 mg zebeta mastercard arrhythmia pac. Hypomagnesemia may also be observed and should be corrected as this may hasten the normalisation of serum ionised calcium zebeta 5mg with amex hypertension 14080. This now appears to be false zebeta 10mg with amex arteriovenous shunt, and indeed it seems that depriving the gut lumen of nutrients is likely to impair gut mucosal barrier function and exacerbate the problem of translocation purchase zebeta 5mg on-line arteria humana de mayor calibre. In clinical trials it is shown that patients with severe acute pancreatitis can tolerate enteral nutrition delivered either by oral intake or by nasoenteric tube feeding with no adverse effect. Pain is very severe and agonising in acute pancreatitis, so it should be relieved as soon as possible. Moreover pain is frequently accompanied by vasoconstriction which may be harmful to the myocardium and may reduce the blood supply to the pancreas to convert simple oedema to necrosis. Morphine, which is quite effective in relieving severe pain, cannot be given in acute pancreatitis as this causes spasm of sphincter of Oddi. Moreover, administration of morphine is frequently followed by nausea and vomiting. Demerol (Meperidine hydrochloride) in a dose of 50 to 100 mg every 4 hours is considered to be the analgesic of choice because of its anticholinergic action. It may be used in combination with Papaverine (100 mg intravenously) or Nitroglycerine. In only extreme cases bilateral paravertebral splanchnic block or epidural block may be necessary. This can be performed (i) by stopping everything by mouth, (ii) by nasogastric aspiration and (iii) by non-absorbable liquid antacid (preferably a combination of mag nesium trisilicate and aluminium hydroxide as a liquid gel). Cimetidine may be effective as an antacid, (iv) An adequate dose of anticholinergic drug such as probanthine 30 mg every 8 hours or atropine sulphate 0. But its general acceptances is still awaited, (vii) Calcitonin also suppresses pancre atic exocrine and gastric acid secretion, so this drug can also be used. Aprotinin is a specific drug which is being used in this condition with improved prognosis, (viii) Somatostatin is a potent in hibitor of pancreatic exocrine secretion and gastric acid output. This can only be used by continu ous intravenous infusion as its circulating half-life in the blood is less than 3 minutes. Though this drug has been effective in reducing mortality from bile-induced pancreatitis in animal models, however multicentre clinical trials have failed to produce reduction in mortality rate in patients with acute pancreatitis, (ix) Chole- cystokinin-receptor antagonist proglumide has also been proved efficacious in animal models and its use is being investigated in human beings. However recent trials have failed to show any detectable improvement in this condition by using this group of drugs. Some of the deleterious effects of acute pancreatitis are caused by activation of pancreatic proteolytic enzymes and to liberation of biologically active polypeptides similar to bradykinin. The release of trypsin from the affected gland is capable of activating pancre atic Kallikrein another proteolytic enzyme which splits to vasoactive decapeptide Kallidin from a globulin. An antienzyme preparation shown to be effective toward trypsin and Kallikrein in both experimental and human acute pancre atitis is Trasylol (Aprotinin). But it should be remembered that once the ne crotic process is well established Trasylol becomes ineffective. So Trasylol has to be used at the earliest possible opportunity in a massive dose (1,00,000 units or more daily intravenously). Recent studies however have failed to show any significant improvement in the condition of patients with acute pancreatitis by using this group of drugs. Although the initial study of aprotonin showed evidence of benefit, several subsequent randomised studies have failed to con firm this. Studies of therapy aimed at inhibiting pancreatic secretion with anticholinergic agents or inhibitory hormones such as glucagon, somatostatin or somatostatin analogues, have all yielded negative findings. There is in fact nothing to demonstrate any effect of octreotide in over 400 patients. The incidence of infec tion is 20% in first week, 40% in second week and 60% in the 3rd week. The or ganisms responsible for infection traverse by translocation from intact gut and are the enteric flora mostly coliform, with 20 to 30% anaerobes. Imipenem is the antibiotic of choice, as (i) it has the maximum blood-pancreas diffusion and (ii) it has widest spectrum against organisms of enteric flora and anaerobes. The next best choice is quinolone (especially ofloxacilin) as the previous drug is quite expensive. Use of these prophylactic antibiotics have significantly reduced the incidence of pancreatic sepsis. It will counteract superimposed infection, prevent widespread peritonitis and suppurative complications. Third generation Cepha losporin has also been claimed to be highly successful in fulmination pancreatitis. It is definite that antibiotic is quite effective against the infective complications of acute pancreatitis. What is not known is the most appropriate antibiotic to be used, and the appropriate duration of therapy. The organisms which infect pancreatic necrosis are usually enteric bacteria and in this respect cefuroxime is a relatively inexpensive, widely available and safe antibiotic which can destroy this bacteria. Attempts to improve pancreatic perfusion with dextran have proved certain beneficial effect in experi mental animals, though not in human beings. Its use is limited to those who continue to deteriorate inspite of the best conservative treatment and when the diagnosis is absolutely confirmed. A lower midline or left lower quadrant incision is used and the peritoneal lavage catheter is introduced by making a nick through the abdominal muscles. This fluid is then drained out by lowering the bottle to the floor in the next 90 minutes. Cardiovascular and respiratory monitoring are imperative as introduction of this fluid into the abdominal cavity may have adverse effects on the cardiac output and pulmonary compliance. Various studies have suggested that peritoneal lavage may be of benefit in reducing the early systemic complication of severe pancreatitis, though further study is required to know specifically the advantage of peritoneal lavage. Use of this drug can reduce the severity of organ failure and also reduce the numbers of patient with local complications. It has shown a significant reduction in mortality rate in the lexipafant treated group. There is some experimental evidence which suggests that Interleukin 10 can diminish the severity of acute pancreatitis. Many conditions of acute abdomen resemble acute pancreatitis and some of them require immediate operation. So doubt in the diagnosis is the first indica tion of surgery in acute pancreatitis. Some conditions very much mimic acute pancreatitis — these are perforated viscus and acute mesenteric ischaemia. As soon as the abdomen is opened, any ascitic fluid, if present, is sampled for amylase, lipase, cell counts, aerobic and anaerobic culture. If this is not detected, the gastrocolic omentum is opened to fully expose the body and tail of the pancreas. In case of severe pancreatitis with large amount of peritoneal fluid exudate peritoneal dialysis catheter is placed, the abdomen is closed and postoperative lavage is contin ued.