Kenyon College. I. Murak, MD: "Purchase cheap Olmesartan online - Cheap Olmesartan online no RX".
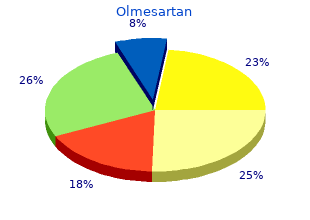
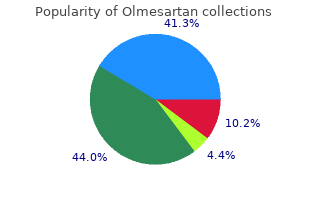
If the swelling is disturbing olmesartan 40mg line blood pressure monitor walgreens, excision may be advised alongwith postoperative thyroxin therapy generic olmesartan 40mg with visa hypertension of chronic kidney disease is medicated with, if there is absence of normal thyroid buy 20 mg olmesartan fast delivery blood pressure medication increased urination. Usually this tract disappears buy cheap olmesartan 40 mg online blood pressure risks, but occasionally it may persist and ultimately a cyst or fistula may develop from this tract which is known as thyroglossal cyst or thyroglossal fistula. But it may be seen just above the hyoid bone or in front of the thyroid cartilage. When it is presented with infection and abscess formation, incision and drainage is the treatment of choice. Once infection is controlled, it should be treated by complete excision usually with removal of central portion of the hyoid bone. The opening of the fistula also varies in position from just above the hyoid bone upto the isth mus of the thyroid. Thyroglossal fistula is lined by columnar epithelium and serous secretion is discharged. The treatment is excision of the whole thyroglossal tract through the central core of lingual muscles. The operation for excision of thyroglossal tract is known as Sistrunk’s operation. It is always advisable to excise middle of the body of the hyoid bone as thyroglossal tract is very closely related to this bone. They descend along with the thyroid and continue to remain in close association with the upper portion of the posterior aspect of the two lateral lobes of the thyroid. Occasionally they may descend as far as the superior portion of the posterior mediastinum and it must be remembered that when they descend to the mediastinum they always lie posterior to the inferior parathyroids. The two inferior parathyroids arise from the third branchial pouch alongwith the thymus and descend during the foetal life with the thymus. These positions are variable starting from below the mandible to the level of the heart. They usually lie in the lower part of the posterior aspect of the two lateral lobes of the thyroid either within the thyroid capsule or outside it or even outside the pretracheal fascia. They may descend from their normal positions to the superior mediastinum and even to anterior mediastinum upto the pericardium. But it must be remembered that they are almost always supplied by the inferior thyroid arteries. These usually lie between the posterior borders of the lobes of the thyroid gland and its capsule. Usually they are 4 in number, two on each side and are called from their positions, the superior and inferior parathyroids. There is an anastomotic artery connecting the superior and inferior thyroid arteries and runs along the posterior border of the lobe of the thyroid gland. The superior parathyroid gland is more constant in position and is usually situated at the middle of the posterior border of the thyroid gland. Hie superior parathyroid glands are usually supplied by the anastomotic artery connecting the superior and inferior thyroid arteries while the inferior parathyroid glands are supplied by the inferior thyroid artery. Only occasionally the inferior parathyroids when they lie abnormally in the mediastinum may receive supply from thymic vessels, internal mammary vessels or rarely from the aorta. In children the gland consists of columns or cords of the principal cells (or chief cells). There are three varieties of chief cells according to the depth of staining — (a) dark chief cells, (b) light chief cells and (c) clear chief cells in which the cytoplasm is not easily stained. At about 10 years of age other cells appear — which are called oxyphil or eosinophil cells. The chief cells are concerned with secretion of parathormone, whereas the function of oxyphil cells is not known. The oxyphil cells are larger than the chief cells and contain more cytoplasm which stains deeply with eosin. The plasma calcium, normally about 10 mg/100 ml is partly bound to protein and partly diffusible. It is the free, ionized calcium which is necessary for coagulation, cardiac and skeletal muscle contraction and nerve function. Calcium in the bone is of two types — (i) readily exchangeable reservoir and (ii) stable calcium what is only slowly exchangeable. Excess dietary calcium is excreted in the stools, but most of the calcium liberated during bone resorption is excreted in the urine. In Vitamin D deficiency the protein matrix of new bone fails to mineralise producing rickets in children. In the kidney, this hormone decreases calcium clearance and causes increased excretion of phosphate in the urine. The latter action is due to inhibition of reabsorption of phosphate from the proximal convoluted portion of the renal tubule. Decrease in tubular reabsorption of phosphate causes phosphaturia and low plasma phosphate level. In the skeleton, parathyroid hormone promotes release of calcium from the bone by active transport process. It stimulates osteoclastic activity and may even convert osteoblasts to osteoclasts. In gastrointestinal tract, this hormone has a direct stimulatory effect on intestinal absorption of calcium. When the calcium level is high, secretion is diminished and calcium is deposited in the bones. When the calcium level is low, the secretion is increased and calcium is mobilized from the bones. There is no trophic hormone which influences the secretion of parathyroid hormone. In conditions such as chronic renal disease, in which the plasma calcium is chronically low, feed-back stimulation of the parathyroid glands causes compensatory parathyroid hypertrophy and secondary hyperparathyroidism. Multiple pancreatico duodenal neuroendocrine tumours causing Zollinger-Ellison syndrome in approximately 50% of cases which may be benign or malignant. There is also benign pituitary adenoma which may be functioning or non-functioning in 40% of cases which may cause acromegaly or cushing’s syndrome or there may be hyperplasia of the adrenal cortex and carcinoid tumour. Other associated disorders include thyroid neoplasms (adenoma or differentiated thyroid carcinoma), adrenal neoplasms and lipomas. In this case there is medullary carcinoma of the thyroid with pheocromocytoma and hyperparathyroidism. In type 2a hyperparathyroidism is seen in 25% of patients, whereas in type 2b there are additional neurofibromas affecting lips, eyelids and face producing swellings in these regions, megacolon and ganglioneuromatosis.
Additional information:
Note the cortical thinning of all bones with evidence of previous pronounced narrowing of the joints involving the talus and fractures and resultant deformities olmesartan 40 mg line arrhythmia band. Radio- graphic signs suggestive of hemophilia include abnormally large or prematurely fused epiphyses purchase olmesartan 10 mg blood pressure chart stress, widening and deepening of the intercondylar notch of the femur cheap 40mg olmesartan fast delivery blood pressure upon waking up, and squaring of the inferior border of the patella generic 10 mg olmesartan with visa arrhythmia jantung. Idiopathic juvenile Rare condition characterized by the abrupt onset osteoporosis of generalized or focal bone pain in children 8 to12 years of age. The disease is usually self- limited with spontaneous radiologic and clinical improvement. Diffuse widening of the muscle bundles, makes the fascial sheaths appear as thin metacarpals and phalanges with thin cortices and coarsened trabeculae. Most common in premature infants and usually develops between 6 and 12 months of age. Classic radiographic signs include cupping and fraying of metaphyseal ends of bone with disappearance of normally sharp metaphyseal lines; delayed appearance of epiphyseal ossification centers, which have blurred margins (unlike the sharp outlines in scurvy); and excessive osteoid tissue in the sternal ends of ribs producing characteristic beading (rachitic rosary). Malabsorption states Primary small bowel disease (sprue, Crohn’s dis- ease, lymphoma, small bowel fistula, amyloidosis); pancreatic insufficiency (exocrine) or inflammation; hepatobiliary disease (biliary atresia or acquired chronic biliary obstruction); postoperative gastric or small bowel resection; mesenteric disease; ca- thartic abuse. This can lead to cation wasting (calcium and potassium) and so-called “renal rickets. Vitamin D–resistant rickets Hereditary disorder (X-linked dominant) with diminished proximal tubular resorption of phos- phorus. Fanconi’s syndrome Multiple defects of renal tubular resorption that may be inherited (autosomal recessive) or acquired secondary to such conditions as Wilson’s disease, multiple myeloma, and lead or cadmium intoxi- cation. Characterized by hypophosphatemia and large amounts of glucose, amino acids, and protein in the urine. Hyperparathyroidism Excessive secretion of parathyroid hormone leads (Fig B 3-3) to a generalized disorder of calcium, phosphorus, and bone metabolism resulting in elevated serum calcium and phosphate. May be primary (adenoma, carcinoma, or generalized hyperplasia of all glands; parathormone-like secretion by nonparathyroid tumor) or secondary (more common and most often due to chronic renal failure). Classic radiographic signs include subperiosteal bone resorption, generalized osteosclerosis (including rugger-jersey spine), brown tumors, salt-and- pepper skull, and soft-tissue calcification. Increased incidence of nephrocalcinosis, urinary tract calculi, pancreatitis, peptic ulcer, and gallstones. Striking thickening of the cortices of the vertebral bodies with increased trabeculation of spongy bone. Hypo- phosphatasia discovered in utero or during the first few days of life is generally fatal, with the calvarium and many bones of the skeleton uncalcified. If the condition develops later, the radiographic appearance closely resembles that of rickets with large unossified areas in the skull simulating severe widening of sutures. Wilson’s disease Rare familial disorder in which impaired hepatic (Fig B 3-5) excretion of copper results in toxic accumulation of the metal in the liver, brain, and other organs. Anticonvulsant drug therapy Prolonged use of anticonvulsants (eg, dilantin) and many tranquilizers stimulates hepatic en- zymatic activity, resulting in accelerated degra- dation of biologically active vitamin D3 to inactive metabolites. Fibrogenesis imperfecta Extremely rare conditions of older individuals and axial osteomalacia in which acquired vitamin D resistance leads to osteomalacia in both the axial and appendicular bones (fibrogenesis imperfecta) or only the axial skeleton (axial osteomalacia). Views of (A) the chest and (B) the abdomen show generalized bony demineralization with striking prominence of residual trabeculae (especially in the ribs). Osteomalacia of the arm with ossification of the deltoid and other muscle insertions. Severe manifestations of the condition in a 43-year-old man, 4 feet 9 inches tall. Lateral view of the ankle and foot demonstrates marked demineralization, thinning of the cortex, and coarsening of the trabecular pattern, all best seen in the os calcis. Almost that most commonly occur in the pelvis and half enlarge over a period of years and many upper femurs. Sharply demarcated lesion, show activity on radionuclide bone scans (must be though the margins often display thorny distinguished from osteoblastic metastases). Osteomas (often multiple) arises in the outer table of the skull, paranasal are associated with soft-tissue tumors and sinuses (especially frontal and ethmoid), and multiple premalignant colonic polyps in Gardner’s mandible. Osteoid osteoma Small, round or oval lucent nidus (less than Benign bone tumor that usually develops in young (Fig B 4-1) 1 cm in diameter) surrounded by a large, dense men. Classic clinical symptom is local pain that is sclerotic zone of cortical thickening. Surgical excision of the nidus is essential for cure (it is not necessary to remove the reactive calcification). Osteoblastic metastases Single or multiple ill-defined areas of increased Osteoblastic metastases are most commonly (Figs B 4-2 and B 4-3) density that may progress to complete loss of secondary to lymphoma and carcinomas of the normal bony architecture. Other primary tumors include isolated round focus of sclerotic density to a carcinomas of the gastrointestinal tract, lung, diffuse sclerosis involving most or all of a bone and urinary bladder. As the lesion that probably represents a local dysplasia of grows, the pull of neighboring muscles and cartilage at the epiphyseal growth plate. The lesion tendons orients the tumor parallel to the long arises in childhood or adolescence and continues axis of the bone and pointed away from the to grow until fusion of the closest epiphyseal line. Typically there is blending of Most commonly develops in the metaphyseal the cortex of an osteochondroma with that of region of a long bone (eg, femur, tibia, or humerus). In flat bones, an osteochondroma Rapid growth or the development of localized pain appears as a relatively localized area of amor- suggests malignant degeneration to chondro- phous, spotty calcification. There are multiple and bilateral osteo- chondromas in hereditary multiple exotoses (diaphyseal aclasis). Multiple areas of increased density involving the pelvis and proximal femurs representing metastases from carcinoma of the urinary bladder. Underlying causes include occlusive vascular (Fig B 4-7) May be sharply limited by a dense sclerotic disease, sickle cell anemia, collagen disease, chronic zone or be associated with serpiginous dense pancreatitis, Gaucher’s disease, and radiation streaks extending from the central region of therapy. Extensive cartilaginous calcification tumor is parallel to that of the femur and pointed away from about the proximal fibular lesion. Densely calcified area in the medullary cavity chondrosarcoma from one of the many exostoses in this of the humerus with dense streaks extending from the central patient appears as a large soft-tissue mass with amorphous region. May articular end of bone areas with flattening and irregularity of joint affect the proximal half of the navicular after a (Fig B 4-8) surfaces leading to early secondary degener- fracture. Also can occur in any disorder associated ative changes (especially in weight-bearing with medullary bone infarcts or be secondary to joints). Healed or healing benign Initially lytic bone lesion may become sclerotic Fibrous cortical defects, nonossifying fibromas, and bone lesion spontaneously or with appropriate therapy. Brown tumors in primary hyperparathyroidism become sclerotic after removal of the parathyroid ade- noma. Even some lytic metastases may become osteoblastic after irradiation, chemotherapy, or hormone therapy. Osteomyelitis Chronic or healed Thickening and sclerosis of bone with irregular Reactivation of infection may appear as recurrence osteomyelitis outer margin surrounding a central ill-defined of deep soft-tissue swelling, periosteal calcification, (Fig B 4-9) area of lucency. The cortex may become so or the development of lytic abscess cavities in the dense that the medullary cavity is difficult to bone.

Considering the fact that the patients do not survive long and in these cases there is high operative mortality buy generic olmesartan 20 mg blood pressure 220, only few patients develop blood borne metastasis order 10 mg olmesartan with mastercard blood pressure chart athlete. Systemic spread is mainly to the liver and lungs generic 40 mg olmesartan visa blood pressure medication in liquid form, but prac tically any organ may be involved including the bone order olmesartan 20 mg arteria heel, brain and skin. Onset is usually insidious and in the beginning nonspecific symptoms like retrosternal discomfort, indigestion, weight loss, occult mild anaemia may be present. At the initial stage dysph agia is more felt during ingestion of solids, but gradually swallowing of liquids and saliva become difficult. Patients may present with rather non-specific dyspeptic symptoms or a vague feeling that something is obstructing during swallowing. Hoarseness due to recurrent nerve palsy is a sign of advance and incurable disease. If the lymph nodes are palpable in the neck, it is also a sign of advanced disease. This can be made with a high degree of accuracy by the usual barium oesophagogram. One may use air-contrast radiographic techniques to detect small lesions of 10 mm diameter, (i) Irregular mucosal filling defects, (ii) distortion of the oesophageal lumen, (iii) annular stricture and (iv) irregular ‘rat-tail’ filling defect of the distal oesophagus may be detected in barium studies. It must be remembered that irregular filling defect more often signifies malignant lesion rather than the smooth, tapered stricture which signifies a benign lesion. The other characteristic feature is that in benign obstructing lesion there is proximal dilatation of the oesophagus of varying degree, but such dilatation is not seen in malignant lesions. Oesophageal biopsy and brushing for cytological examination may be performed through oesophagoscopy. Bron choscopy may be performed when the lesion involves upper oesophagus to detect malignant in volvement of the adjacent tracheobronchial tree. Additional diagnostic study such as radioactive phosphorus which is concentrated in the carcinomas is not so popular. Bronchoscopy should be done particularly in lesions of the upper and middle-thirds where there may be tracheal and bronchial invasion. Mediastinoscopy is important to know involvement of mediastinal group of lymph nodes. Laparoscopy is particularly important in case of adenocarcinoma of the distal oesophagus to detect transperitoneal spread and liver metastasis. Respiratory and cardiovascular function are the most important aspects to assess the patients before operation. In these cases double contrast barium study of the oesophagus is a highly sensitive modality for diagnosing early and advanced carcinoma of the oesophagus. But barium studies can neither evaluate the depth of invasive growth nor assess the exact length of tumoural lesion within the oesophagus. Involvement of the trachea and main stem bronchus should be suspected if an oesophageal cancer either causes inward bowing of the posterior tracheal or bronchial wall or dis places the trachea and/or bronchi away from the spine. The average 5 years survival rate following radiotherapy is less than 10% and not more than 17% even in the reported series of its strongest proponent. Radical radiation therapy is also associated with complication such as radiation pneumonitis, post radiation stricture, tracheo-oesophageal fis tula, spinal cord injury, pericardial effusion and constrictive pericarditis. Palliative low dose radiotherapy (2,000 to 3,000 rads) may be used to alleviate distressing symptoms such as pain, dysphagia and bleeding. Preoperative radiation appears to improve resectibility, though its application is yet not popularised. In case of cancers affecting upper two-thirds of the oesophagus radical surgery is not possible in majority of cases and surgery is mainly aimed at palliation so that the patient can eat properly during the rest of his life. Operative mortality is approximately 25% and 3 years survival rate is approximately 25% to 35%. In cervical growths the treatment of choice still remains radiotherapy and surgery as yet has not made any appreciable advances. Accessibility of the lesion, its lymphatic field and all adjacent structures have made block dissection of the growth possible. Growth at this part of the oesophagus should be further subdivided into (a) Infradiaphragmatic cancers and (b) Supradiaphragmatic cancers. In the beginning only medial part of the incision is made to know if the tumour is inoperable or not. The stomach alongwith its whole lymphatic field the spleen, lower third of oesophagus and even left lobe of the liver are excised. Reconstruction using Roux-en-Y jejunal loop with jejuno-jejunum anastomosis should be performed. In case of oesophago-jejunal anastomosis there is chance of biliary regurgitation, heart bum and stricture formation. In this technique upper left paramedian incision is made and the stomach is mobilised carefully to preserve its blood supply from gastroepip loic arch and the right gastric artery. The left gastric artery is secured close to its origin and smaller vessels in the region of the diaphragmatic hiatus are divided. Pyloromyotomy as performed in Ramstedt’s operation is carried out since oesophageal resection will cause complete trunkal vagot omy and pyloromyotomy will help in proper emptying of the stomach. The right side is preferred as no important great ves A B sels intervene in mobilisation of the oe sophagus. The opening in the stomach being cresentic in shape on theanterior wall of the stomach adequate distance away from the stapled suture line. This part should be divided into (a) lower half and (b) upper half for better description. Moreover cardiac, aortic and pulmonary movements make accurate insertion of suture difficult and the anastomosis may be unsound with subse quent leakage. To avoid the dangers of per forming anastomosis in the depth of the thoracic cavity, the method of total oesoph- Fig. But this technique did not stand due to fistula formation and non-acceptance of a good anastomosis between the high columnar epithelium of jejunum and squamous epithelium of upper oesophagus. Subsequently transverse colon, right colon or even left colon was used in front and behind sternum to bridge the gap between cervical oesophagus and the stomach. But again leakage and stricture formation appear to be the common complications after these types of replacement. Ultimately three-stage oesophagectomy bringing the stomach as a whole up into the neck and anastomosing with the cervical oesophagus was introduced. This technique otherwise became successful as this is a more physiological approach by making anastomosis between the oesophagus and the stomach. In this technique the first two stages are similar to those of Lewis-Tanner procedure. Each omental branch of the gastroepiploic arch is ligatured separately and not by bunching.