Westminster College, Salt Lake City. A. Nemrok, MD: "Buy Aurogra no RX - Safe online Aurogra".
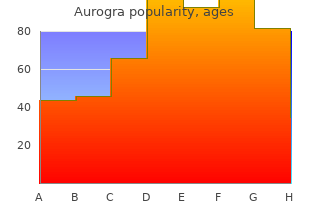
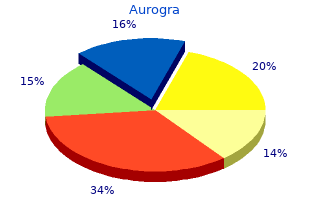
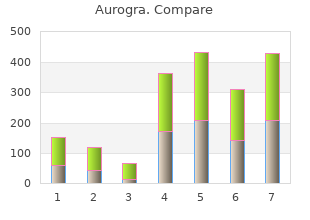
Extensive necrosis involving the whole esophagus First degree Mucosal inflammation generic 100mg aurogra free shipping erectile dysfunction uptodate, edema cheap 100mg aurogra with mastercard erectile dysfunction definition, or superficial sloughing Second degree Damage extends to all layers of buy generic aurogra 100 mg online impotence 101, but not through buy discount aurogra 100mg line erectile dysfunction doctor type, the esophagus Third degree Ulceration through to periesophageal tissues p. Cineesophagography can detect esophageal motility disorders, the pattern of which may predict the likelihood of stricture formation. Strictures can be expected to develop in all patients with an atonic dilated or rigid esophagus and in some individuals with abnormal, uncoordinated contractions [39]. Computed tomography may have a role in the evaluation of caustic injury, but current evidence suggests endoscopy is preferred [41]. Esophageal motility studies may predict the risk of stricture formation in those patients with no peristaltic response; these motility abnormalities persist for at least 3 months [42]. Evaluation of patients with symptoms and signs of systemic toxicity should include routine monitoring and ancillary testing. The extent and type of testing depend on the nature and severity of clinical abnormalities and the chemical involved. Treatment of systemic poisoning is primarily supportive; in some cases, antidotal therapy may also be necessary. The persistence of eye pain despite irrigation for at least 15 minutes indicates significant injury or incomplete decontamination. Failure to irrigate the eye adequately or remove particles after chemical exposure is associated with chronic complications [43]. Up to one-third of patients with lime burns still have particles present in the eye on presentation [43]. Ascorbic acid had been used to treat alkali burns, but its effectiveness has not been well studied, and it cannot be recommended [12]. The initial treatment of dermal exposure is prompt irrigation with copious amounts of water for at least 15 minutes for acid exposures and 30 minutes for alkali. Although tissue neutralization occurs within 10 minutes with acids and within 1 hour with alkalis in experimental studies, delayed irrigation may be beneficial [44]. Clothes act as a reservoir, and failure to remove them may result in full- thickness burns developing from even mildly corrosive chemicals. Neutralization has been associated with good outcomes [45], but because systematic data on its efficacy are lacking, such therapy cannot be recommended. Metallic lithium, sodium, potassium and cesium, titanium tetrachloride, and organic salts of lithium and aluminum react violently with water; burns caused by these agents should be inspected closely and any particles removed and placed in an anhydrous solution (oil) before the area is irrigated. Alternatively, the area can be wiped with a dry cloth to remove particles and the skin then deluged with water to dissipate any heat. Phenol is not water soluble, and dilution with water may aid its penetration into tissues, increasing systemic absorption [22]. Soaking experimental phenol burns with isopropyl alcohol or polyethylene glycol in mineral oil is superior to rinsing with water [46]. Isopropyl alcohol and polyethylene glycol may be absorbed by burns, and their use should be followed by liberal washing with water. A report describes removing ready-mixed concrete from skin by soaking or irrigating with 50% dextrose in water [47]. Application of a copper sulfate solution has been suggested to assist in identification and neutralization of white phosphorus particles on the skin, but systemic absorption of copper sulfate can result in massive hemolysis with acute renal failure and death [48]. British antilewisite, or dimercaprol, is an effective chelator of lewisite and can be applied topically to the skin or eye [16]. Definitive management is the same as for thermal burns, although more aggressive use of early débridement and grafting has been suggested [15]. Dilution by drinking up to 250 mL (120 mL for a child) water or milk is recommended for particulate ingestion, because the corrosive may adhere to the esophageal wall. Because the efficacy of dilution is greatest if performed within 5 minutes of exposure and declines rapidly thereafter, it is reasonable to use any drinkable beverage, except carbonated ones, if water or milk is not immediately available. It may, however, promote emesis and may not be effective in limiting tissue damage unless undertaken within minutes of injury. Emesis is contraindicated because of the risk of aspiration and its association with an increased severity of esophageal and laryngeal burns [19]. The administration of weak acids or bases can neutralize, as well as dilute, ingested corrosives [37]. Although weak acids are more effective than milk or water in neutralizing the pH, neutralization, which is accompanied by the production of heat, could lead to thermal injury in addition to corrosive effects. The heat generated by in vitro neutralization is small (less than 3°C) for liquid alkali but may be greater for solid forms [37]. Using a nasogastric tube for gastric aspiration, dilution, or lavage is another subject of debate [6]. Esophageal perforation is a potential complication, but no cases of nasogastric tube perforation have been reported. Placement of a gastric tube with fluoroscopic or endoscopic guidance has been suggested, but the blind, gentle introduction of a small-bore tube in a cooperative patient, particularly for a large acid ingestion, also appears to be safe [17]. In addition, because it interferes with endoscopic evaluation, unless a corrosive has a significant systemic toxicity and is known to be bound by activated charcoal, this agent should be avoided. Corticosteroids have been used to reduce the incidence and severity of esophageal strictures after alkali burns. Such therapy is based on studies showing a decrease in stricture formation in animals pretreated with steroids [50]. Because strictures do not develop in patients with first- degree esophageal burns, steroids are not indicated in those with such findings [51]. Similarly, steroids do not appear to influence the development of esophageal strictures after extensive deep ulceration or necrosis [51], and hence they are not recommended in patients with these injuries. Studies on the efficacy of steroids in patients with injuries of moderate severity have yielded conflicting results. There have been four prospective controlled studies comparing steroids to placebo for prevention of strictures. An older small study suggested a small decrease in the percentage of patients who will develop esophageal strictures [54]. A recent well-designed study found a 20% decrease in strictures and a decrease in the need for 2 parenteral nutrition with high-dose methylprednisilone (1 g/1. One comparative study suggested a 30% absolute risk reduction in risk of stricture with dexamethasone (1 mg per kg per day) compared with prednisolone (2 mg per kg per day) [55]. Overall, the data are inconclusive, and no definitive recommendations on the effectiveness of steroids can be provided. Although prior recommendations suggested that therapy should be continued for at least 10 days [51], the most recent study suggests that 3 days of high-dose methlyprednisilone is effective. Patients with no injury or mucosal inflammation or small areas of superficial ulceration are not at risk for strictures or perforation and require supportive therapy only. Symptomatic relief can be provided with antacids, sucralfate, histamine-2–blockers (H -blockers), or2 analgesics.
Myrobalan Emblic (Indian Gooseberry). Aurogra.
- What is Indian Gooseberry?
- Dosing considerations for Indian Gooseberry.
- Lowering cholesterol and triglyceride levels, cancer, indigestion, eye problems, joint pain, diarrhea, obesity, diabetes, and other conditions.
- How does Indian Gooseberry work?
- Are there safety concerns?
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96763
Agee C cheap aurogra 100 mg online erectile dysfunction caused by low blood pressure, Coulter L aurogra 100mg sale erectile dysfunction and prostate cancer, Hudson J: Effects of pharmacy resident led education on resident physician prescribing habits associated with stress ulcer prophylaxis in non-intensive care unit patients order aurogra 100 mg fast delivery impotence male. Villanueva C generic aurogra 100 mg otc erectile dysfunction doctor in miami, Colomo A, Bosch A, et al: Transfusion strategies for acute upper gastrointestinal bleeding. Although a detailed review of the physiology of motility is beyond the scope of this chapter, it is important for the critical care provider to understand that the closely coordinated movements of the gastrointestinal tract, from mouth to rectum, can frequently be disrupted and deranged in the setting of severe illness. Rather, physiologic reserve shifts away from the gastrointestinal tract to critical organs such as the lungs, brain, and cardiovascular system, resulting in significant dysfunction and possibly damage of the gastrointestinal tract. This presents most often as delayed transit, or ileus, which may occur at any level of the gastrointestinal tract leading to a number of clinically significant consequences such as gastroesophageal reflux, gastroparesis, abdominal pain and distention, obstipation, and even bowel ischemia and perforation. Because derangements of gastrointestinal motility are extremely prevalent in the critically ill, providers must be prepared to identify and treat these morbid, and sometimes fatal disorders. Although there has been surprisingly little research dedicated to understanding the pathophysiologic basis of motility abnormalities in the critically ill patient [1], there have nonetheless been several advances in the prevention and treatment of these disorders. First, critically ill patients are often in the recumbent position, which promotes acid reflux [4–6] and reduces acid clearance from the esophagus. Second, many critically ill patients are intubated, sedated, or too ill to report symptoms of acid reflux, which can thus go unrecognized until complications occur. Fourth, critically ill patients often develop concomitant gastroparesis (see following discussion) from a host of factors, which, in turn, favors retrograde flow of gastric contents toward the distal esophagus. Taken together, these multiple mechanisms concur to clinically significant acid reflux and to its related complications. Several nonpharmacologic steps should be taken in the critical care setting to minimize complications of acid reflux in the critically ill patient. This maneuver can minimize acid stasis in the distal esophagus and improve emptying of stomach contents, thereby reducing complications of acid reflux [4,5]. The effectiveness of this maneuver alone for patients who are mechanically ventilated remains controversial [5,6]. Patients with gastroparesis typically present with nausea, vomiting, abdominal pain, early satiety, and postprandial bloating. These symptoms can be blunted or overlooked during critical illness, given the severity of the overall clinical picture and the concomitant treatments. Because the symptoms of gastroparesis are often nonspecific, the clinician should maintain a low threshold for considering the diagnosis. A combination of physical examination findings and imaging studies confirm gastroparesis and exclude competing diagnoses, including mechanical obstruction and mucosal diseases. On examination, patients with gastroparesis may demonstrate epigastric distention with tenderness but typically lack abdominal rigidity or guarding, signs of a potentially more serious acute diagnosis. The examiner should evaluate for a succussion splash by placing the stethoscope over the left upper quadrant while gently shaking the abdomen laterally by holding either side of the pelvis. A positive test occurs when a splash is heard over the stomach and favors the diagnosis of mechanical gastric outlet obstruction over gastroparesis. Of note, the maneuver is only valid if the patient has not received solids or liquids within the previous 3 hours. Serum electrolyte levels, serum glucose level, hemoglobin A1C level, serum cortisol level, thyroid-stimulating hormone level, amylase, and white blood cell count (screen for infection) should be measured. Plain films of the abdomen should be obtained to evaluate for evidence of gastric distention and to screen for overt evidence of gastric obstruction. Upper endoscopy should be considered if there is suggestion of gastric outlet obstruction, because significant amounts of retained food, feedings, and secretions can be found in the stomach even in the absence of an obstruction to the pyloric outlet. Formal measurement of gastric motor function is impractical and not routine in the critical care setting. The most accepted diagnostic test, usually performed in the outpatient setting, is a scintigraphic emptying study. Still, the simple finding of persistent high gastric tube residuals should be sufficient to formulate a presumptive diagnosis in the critically ill patient. Once diagnosed, a search for possible reversible causes of gastroparesis (including mechanical obstruction and medications) should be undertaken. Treatment should begin by with nutritional and dietary modifications including smaller volume, low-fat, and low-fiber meals or tube feeds [20]. Consultation with the nutrition or metabolic support services is often warranted to help select between available liquid caloric supplements. Rather, patients who need long-term nutrition support due to gastroparesis should be considered for a jejunostomy tube [21], often placed in conjunction with a gastrostomy tube for venting of the stomach [22]. Metoclopramide and erythromycin are the only currently available prokinetic medications in the United States. Other prokinetics available outside the United States include domperidone, prucalopride, and mosapride. Metoclopramide has multiple actions, including coordination of antral, duodenal, and pyloric muscle function, while simultaneously serving as a centrally acting antiemetic [23,24]. Subcutaneous dosing (two to four times per day in 2-mL aliquots) has been promoted as an alternative route, as it is associated with more stable plasma levels [25]. Other neurologic side effects include akathisia, sedation, and depression, can impact up to 30% of patients [26]. Erythromycin may be used in combination with metoclopramide for patients with an incomplete response to either 13 agent alone. Oral dosing of erythromycin (125 to 250 mg twice daily) is effective in diabetic patients and has also shown benefits in reducing high tube feed residuals [30]. Unfortunately, long-term use of erythromycin leads to tachyphylaxis from downregulation of motilin receptors [28] and also is associated with antimicrobial resistance. However, this treatment is available at only limited centers and is rarely used in critically ill patients. Pyloric botulin toxin injection has not been shown to be effective in gastroparesis and its role in the critically ill patient is unknown [31]. However, pharmacologic agents with adequate selectivity and bioavailability are currently not available and still under investigation [32]. Patients typically present with abdominal distention, obstipation, nausea, vomiting, abdominal pain, and high tube feed residuals. Distinguishing ileus from small bowel obstruction is critical, as prolonged mechanical obstruction can lead to bowel ischemia and peritonitis. Peritoneal signs and auscultation of high-pitched bowel sounds favor small bowel obstruction, whereas a silent bowel suggests ileus. Although the skilled clinician often can reliably distinguish small bowel obstruction from ileus on the basis of history and physical examination alone, plain abdominal radiographs may serve to confirm the clinical impression. Ileus typically is characterized by the presence of both small and large bowel dilatation, the presence of gas throughout the bowel and into the rectum, lack of a luminal radiographs may serve to confirm high pitched bowel sounds, small bowel obstruction typically presents with small bowel distention in the absence of colonic gas, a paucity of gas in the rectum, air fluid levels on upright positioning, and with evidence of a luminal transition point. Despite the stereotypical features of small bowel obstruction and ileus, plain film imaging does not always provide a definitive diagnosis, as long- standing ileus or partial small bowel obstruction may appear similar on abdominal imaging. In addition, late-stage mechanical obstruction may lead to exhaustion of intestinal propulsive activity, resembling adynamic ileus without high-pitched bowel sounds and a similar air distribution pattern on plain abdominal X-rays. Common causes in the critically ill patient include electrolyte abnormalities, sepsis, inflammation, postoperative hypomotility, and medications (Table 205.
Nausea and diarrhea are the most common adverse effects of lubiprostone (ure 38 buy aurogra 100mg fast delivery erectile dysfunction how common. Misoprostol interacts with prostaglandin receptors on parietal cells within the stomach generic aurogra 100 mg with mastercard coffee causes erectile dysfunction, reducing gastric acid secretion cheap aurogra 100 mg with visa erectile dysfunction drugs new. Its use is limited by common adverse effects including diarrhea and abdominal pain purchase aurogra 100mg otc erectile dysfunction grand rapids mi. By binding to prostaglandin receptors, they increase uveoscleral outflow, reducing intraocular pressure. They are administered as ophthalmic solutions once a day and are as effective as timolol or better in reducing intraocular pressure. Bimatoprost increases eyelash prominence, length, and darkness and is approved for the treatment of eyelash hypotrichosis. Ocular reactions include blurred vision, iris color change (increased brown pigmentation), increased number and pigment of eyelashes, ocular irritation, and foreign body sensation. These drugs mimic the effects of prostacyclin in endothelial cells, producing a significant reduction in pulmonary arterial resistance with a subsequent increase in cardiac index and oxygen delivery. Epoprostenol and treprostinil are administered as a continuous intravenous infusion, and treprostinil is administered orally or via inhalation or subcutaneous infusion. Dizziness, headache, flushing, and fainting are the most common adverse effects (ure 38. They act primarily by inhibiting the cyclooxygenase enzymes that catalyze the first step in prostanoid biosynthesis. This leads to decreased prostaglandin synthesis with both beneficial and unwanted effects. Mechanism of action Aspirin is a weak organic acid that irreversibly acetylates and, thus, inactivates cyclooxygenase (ure 38. Anti-inflammatory actions Inhibition of cyclooxygenase diminishes the formation of prostaglandins and, thus, modulates aspects of inflammation mediated by prostaglandins. One exception is ketorolac, which can be used for more severe pain, but for only a short duration. Antipyretic action Fever occurs when the set-point of the anterior hypothalamic thermoregulatory center is elevated. This rapidly lowers the body temperature of febrile patients by increasing heat dissipation through peripheral vasodilation and sweating. For example, two 325-mg aspirin tablets administered four times daily produce analgesia, whereas 12 to 20 tablets per day produce both analgesic and anti-inflammatory activity. Chronic use of aspirin allows for continued inhibition as new platelets are generated. External applications Salicylic acid is used topically to treat acne, corns, calluses, and warts. Methyl salicylate (“oil of wintergreen”) is used externally as a cutaneous counterirritant in liniments, such as arthritis creams and sports rubs. Diclofenac is available in topical formulations (gel or solution) for treatment of osteoarthritis in the knees or hands. In addition, ocular formulations of ketorolac are approved for management of seasonal allergic conjunctivitis and inflammation and pain related to ocular surgery. Aspirin After oral administration, aspirin is rapidly deacetylated by esterases in the body to produce salicylate. Unionized salicylates are passively absorbed mainly from the upper small intestine. Salicylates (except for diflunisal) cross both the blood–brain barrier and the placenta and are absorbed through intact skin (especially methyl salicylate). Salicylate is converted by the liver to water-soluble conjugates that are rapidly cleared by the kidney, resulting in first-order elimination and a serum half-life of 3. At anti-inflammatory dosages of aspirin (more than 4 g/day), the hepatic metabolic pathway becomes saturated, and zero-order kinetics are observed, leading to a half-life of 15 hours or more (ure 38. Therefore, aspirin should be avoided in gout, if possible, or in patients taking probenecid. Platelet aggregation is the first step in thrombus formation, and the antiplatelet effect of aspirin results in a prolonged bleeding time. Decreased synthesis of prostaglandins can result in retention of sodium and water and may cause edema. Patients with a history of heart failure or kidney disease are at particularly high risk. These effects can also mitigate the beneficial effects of antihypertensive medications. Approximately 15% of patients taking aspirin experience hypersensitivity reactions. Drug interactions Salicylate is roughly 80% to 90% plasma protein bound (albumin) and can be displaced from protein-binding sites, resulting in increased concentration of free salicylate. Alternatively, aspirin can displace other highly protein-bound drugs, such as warfarin, phenytoin, or valproic acid, resulting in higher free concentrations of these agents (ure 38. Toxicity Mild salicylate toxicity is called salicylism and is characterized by nausea, vomiting, marked hyperventilation, headache, mental confusion, dizziness, and tinnitus (ringing or roaring in the ears). When large doses of salicylate are administered, severe salicylate intoxication may result (see ure 38. Restlessness, delirium, hallucinations, convulsions, coma, respiratory and metabolic acidosis, and death from respiratory failure may occur. Children are particularly prone to salicylate intoxication; ingestion of as little as 10 g of aspirin can be fatal. The dosage should be reduced in those with moderate hepatic impairment, and celecoxib should be avoided in patients with severe hepatic or renal disease. Adverse effects Headache, dyspepsia, diarrhea, and abdominal pain are the most common adverse effects. Patients who are at high risk of ulcers and require aspirin for cardiovascular prevention should avoid the use of celecoxib. Acetaminophen has less effect on cyclooxygenase in peripheral tissues (due to peripheral inactivation), which accounts for its weak anti-inflammatory activity. Therapeutic uses Acetaminophen is used for the treatment of fever and the relief of pain. Acetaminophen is the analgesic/antipyretic of choice for children with viral infections or chickenpox (due to the risk of Reye syndrome with aspirin). It is conjugated in the liver to form inactive glucuronidated or sulfated metabolites. Adverse effects At normal therapeutic doses, acetaminophen has few significant adverse effects.
With an onset of action that ranges from 3 to 36 hours after first dose discount aurogra 100 mg without a prescription impotence only with wife, intranasal corticosteroids improve sneezing trusted 100mg aurogra erectile dysfunction evaluation, itching effective 100mg aurogra impotence with diabetes, rhinorrhea aurogra 100mg visa diabetic with erectile dysfunction icd 9 code, and nasal congestion. To minimize systemic absorption, patients should be instructed to avoid deep inhalation during administration into the nose, because the target tissue is the nose, not the lungs or the throat. For patients with chronic rhinitis, improvement may not be seen until 1 to 2 weeks after starting therapy. When administered intranasally, these drugs have a rapid onset of action and show few systemic effects. However, intranasal formulations of α-adrenergic agonists should be used for no longer than 3 days due to the risk of rebound nasal congestion (rhinitis medicamentosa). For this reason, the α-adrenergic agents are not used in the long-term treatment of allergic rhinitis. Administration of oral α-adrenergic agonists results in a longer duration of action but also increased systemic effects, such as increased blood pressure and heart rate (see Chapter 6). As with intranasal formulations, regular use of oral α-adrenergic agonists (phenylephrine and pseudoephedrine) alone or in combination with antihistamines is not recommended. Other agents Intranasal cromolyn may be useful in allergic rhinitis, particularly when administered before contact with an allergen. To optimize the therapeutic effect, dosing should begin at least 1 to 2 weeks prior to allergen exposure. Although potentially inferior to other treatments, some leukotriene receptor antagonists are effective for allergic rhinitis as monotherapy or in combination with other agents. An intranasal formulation of ipratropium is available to treat rhinorrhea associated with allergic rhinitis or the common cold. Drugs Used to Treat Cough Coughing is an important defense mechanism of the respiratory system in response to irritants and is a common reason for patients to seek medical care. A troublesome cough may represent several etiologies, such as the common cold, sinusitis, or an underlying chronic respiratory disease. In some cases, cough may be an effective defense reflex against an underlying bacterial infection and should not be suppressed. Before treating cough, identification of its cause is important to ensure that antitussive treatment is appropriate. The priority should always be to treat the underlying cause of cough when possible. However, common adverse effects, such as constipation, dysphoria, and fatigue, still occur. In addition, codeine has addictive potential, which limits its use, given increasing concerns with opioid addiction in the United States (see Chapter 14). It has a better adverse effect profile than does codeine and is equally effective for cough suppression. However, it is also a potential drug of abuse, since it may cause dysphoria at high doses. It anesthetizes the stretch receptors located in the respiratory passages, lungs, and pleura. These localized effects may be particularly problematic if the capsules are broken or chewed and the drug comes in direct contact with the oral mucosa. Inhalation of a rapid-acting β agonist, such as albuterol, usually provides immediate2 bronchodilation. An acute asthmatic crisis often requires intravenous corticosteroids, such as methylprednisolone. Inhaled corticosteroids such as beclomethasone and fluticasone treat chronic airway inflammation but do not provide any immediate effect. Propranolol is a nonselective β-blocker and would aggravate the bronchoconstriction. She is now receiving therapy that has greatly reduced the frequency of severe attacks. Administration of an inhaled corticosteroid such as fluticasone significantly reduces the frequency of severe asthma attacks. This benefit is accomplished with minimal risk of the severe systemic adverse effects of oral corticosteroid therapy. Zafirlukast may reduce the severity of attacks, but not to the same degree or consistency as fluticasone (or other corticosteroids). Despite using salmeterol twice daily, he reports continued symptoms of shortness of breath with mild exertion. Roflumilast is not indicated, since the patient only has moderate airway obstruction. Her regimen for the past year has included inhaled salmeterol twice daily and inhaled tiotropium once daily. The addition of an inhaled corticosteroid may provide additional benefit since the patient has significant airway obstruction and frequent exacerbations requiring hospitalization. It is not routinely recommended to discontinue a long-acting bronchodilator unless the patient experiences an adverse effect or experiences no therapeutic benefit. In this case, the patient reports mild symptoms in between exacerbations, suggesting she may benefit from both bronchodilators. Benzonatate suppresses the cough reflex through peripheral action and has no abuse potential. Dextromethorphan, an opioid derivative, and codeine, an opioid, both have abuse potential. Inhaled corticosteroids have direct anti-inflammatory properties on the airways and require regular dosing to be effective. Salmeterol and albuterol are both bronchodilators, but do not have anti-inflammatory properties. Chlorpheniramine and diphenhydramine are first-generation antihistamines and are usually not a preferred treatment due to their increased risk of adverse effects, such as sedation, performance impairment, and other anticholinergic effects. Cetirizine is a second-generation antihistamine and is generally better tolerated, making it a preferred agent for allergic rhinitis. While zafirlukast and montelukast both inhibit the effects of leukotrienes, they do so by blocking the receptor. Use a large-volume chamber (spacer) to decrease deposition of drug in the mouth caused by improper inhaler technique. Rinse mouth in a “swish-and-spit” method with water prior to inhaler use to decrease the chance of adverse events. Rinsing the mouth may be appropriate for either type of inhaler if the medication being administered is an inhaled corticosteroid; however, this should always be done following inhaler use, not prior to use. Intranasal decongestants should be used no longer than 3 days due to the risk of rebound nasal congestion (rhinitis medicamentosa).
Buy discount aurogra 100mg. 10 Foods That Help Erectile Dysfunction.