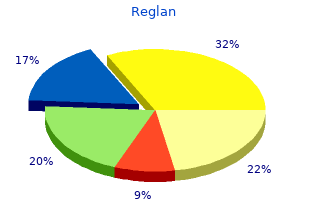
Meredith College. K. Kulak, MD: "Buy Reglan online - Best Reglan online OTC".
Because work can be measured as force x distance cheap reglan 10 mg with amex definition of gastritis in english, the amount of work involved in breathing can be expressed as a change in lung volume (distance) multiplied by the change in transpulmonary pressure (force) discount 10mg reglan amex gastritis diet cheese. With a volume change buy reglan 10mg overnight delivery gastritis diet ôčëüěű, the work involved in taking a breath is defined by this equation: (23) where P equals transpulmonary pressure and ΔV equals change in lung volume reglan 10 mg for sale gastritis diet menu. During work, energy is expended with muscular contraction to create a force (transpulmonary pressure) to inflate the lungs. When a greater transpulmonary pressure is required to bring more air into the lungs, more muscular work and, hence, greater energy are required. In healthy people at rest, the energy needed for breathing represents ~5% of the body’s total energy expenditure. During heavy exercise, about 20% of the total energy expenditure is involved in breathing. Breathing is efficient and is most economical when elastic and resistive forces yield the lowest work. Note that the total inspiratory work of breathing in a restrictive lung disorder, compared with the normal lung, is increased and is a result of a greater inspiratory effort required. It is important to remember that lungs with a marked decrease in lung compliance (i. Patients with a restrictive disorder economize their ventilation by taking rapid and shallow breaths. In contrast, patients with severe airway obstruction tend to do the opposite; they take deeper breaths and breathe more slowly, to reduce their work resulting from the increased airway resistance. Despite this tendency, patients with obstructive disease still expend a considerable portion of their basal energy for breathing. The reason for this is that the expiratory muscles must do additional work to overcome the increased airway resistance. These different breathing patterns help minimize the amount of work required for breathing. His mother reported that Jack had an upper respiratory tract infection for two days and had been using an inhaler more frequently. Today, he has received treatment every three hours, but still complains of shortness of breath and frequent episodes of coughing. His inhaler medication is Flovent (a prescription inhaled corticosteroid medicine for the long-term treatment of asthma in people aged 4 years and older). A call to the pharmacy verifies the correct dosage, and the prescription has been refilled at appropriate interviews. Upon further assessment by the attending resident, Jack’s heart rate was 150; respiratory rate 45; blood pressure 95/65; temperature 37°C; and breathing sounds faint expiratory wheezes throughout all lung fields. The follow discussion will cover the immunology, pathophysiology, pharmacology, etiology, and the treatment of asthma. Asthma is defined as a chronic inflammatory disease of the airways characterized by reversible bronchospasm. There are three main characteristics of asthma: (1) inflammation, (2) hyperresponsiveness, and (3) airway obstruction. In asthma patients, the inflammation is induced by an overreaction to triggers (allergens, pollutants, animal dander, etc. When the airways (bronchi) become hyperresponsive, they have an exaggerated response that leads to bronchospasms. As a result of the inflammation and hyperresponsiveness, asthmatic patient have severely constricted airways. In response to low oxygen, heart and respiratory rate are increased as compensatory mechanism. The cellular mechanism for induced bronchospasms is mast cells degranulation and the release a variety of mediators (histamine, prostaglandins, thromboxane, and bradykinin). The treatment of asthma involves bronchodilators and long-term anti-inflammatory medications. Bronchodilators dilate the bronchi and bronchioles, decrease airway resistance, and increase airflow to the lungs. The bronchodilators are available in inhaled, tablet, liquid, and injection forms, but the preferred method is by inhalation. There three types of bronchodilators: beta agonists (short acting and long acting), anticholinergics (short acting), and theophylline (long acting). Long-term anti-inflammatory medicines are prescribed to prevent asthma attacks and reduce inflammation, swelling, and mucus production. One common side effect from inhaled corticosteroids is thrush (a mouth infection). If taken for long periods, these medications can increase the risk of cataracts and osteoporosis. The alveolar–capillary membrane forms a large blood–gas interface for diffusion of oxygen and carbon dioxide. A negative alveolar pressure is created during inspiration to bring air into the lungs. A positive alveolar pressure is created during expiration to exhaust air out of the lungs. Forced vital capacity is one of the most useful spirometry tests to assess lung function. Minute ventilation is the volume of air expired per minute and is equal to expired minute ventilation. Alveolar ventilation is the amount of fresh air that reaches alveoli and regulates carbon dioxide levels in the blood. Physiologic dead space volume is the portion of tidal volume that is wasted air and does not participate in gas exchange. It is the sum of anatomic dead space volume minus the volume of air in the conducting zone alveolar dead space volume minus volume of air in alveoli that does not participate in gas uptake. Total airway resistance consists of two components: (1) tissue resistance of lungs and chest wall and (2) resistance to airflow in the airways. The work of breathing is required to expand the lungs and overcome airway resistance. Which of the following would best characterize pulmonary function in a patient diagnosed with asthma compared to normal predicted values? Pleural pressure would be the most negative at maximal inspiration (total lung capacity). If carbon production remains unchanged, one hyperventilates for 2 minutes, both alveolar and arterial carbon tensions decrease. Hyperventilation increases oxygen tension in the alveolar but has little effect on arterial oxygen tension. Dead space ventilation = minute ventilation – alveolar ventilation (9 L/minute – 6 L/minute = 3 L/minute).
Zinc The average daily zinc intake is 10 to 15 mg order 10mg reglan with amex gastritis diet ocd, about half of which is absorbed buy reglan 10 mg overnight delivery gastritis diet óęđ, primarily in the ileum purchase reglan 10mg with amex gastritis symptoms breathing. A carrier located in the brush border membrane actively transports zinc from the lumen into the cell reglan 10 mg online gastritis diet brat, where it can be stored or transferred into the bloodstream. Iron Iron plays an important role not only as a component of heme but also as a participant in many enzymatic reactions. Consequently, in the duodenum and upper 3+ jejunum, unless Fe ion is chelated, it forms a precipitate. Several compounds such as tannic acid in tea and phytates in vegetables form insoluble complexes with iron, preventing absorption. Iron is absorbed by an active process via a carrier(s) located in the brush border membrane. One such transporter, the divalent metal transporter, is expressed abundantly in the duodenum. A ferric reductase enzyme on the enterocyte brush border reduces ferric iron Fe to Fe. Once inside the cell, heme iron is released by the action of heme oxygenase and mixed with the intracellular free iron pool. Iron is either stored in the enterocyte cytoplasm bound to the storage protein apoferritin to form ferritin or transported across the cell bound to transport proteins, which carry the iron across the cytoplasm and release it into the intercellular space. Transferrin, a β-globulin synthesized by the liver, binds and transports iron in the blood. Iron absorption is closely regulated by iron storage in enterocytes and iron concentration in the plasma. Enterocytes are continuously shed into the lumen, and the ferritin contained within is lost. In iron deficiency, the circulating plasma iron concentration is low, which stimulates the absorption of iron from the lumen and the transport of iron into the blood. Moreover, in a deficient state, less iron is stored as ferritin in the enterocytes, so the loss of iron through this means is significantly reduced. In iron-loaded patients, there is less absorption of iron because of the large amount of mucosal iron storage, which increases iron loss as a result of enterocyte shedding. Furthermore, because of the high level of circulating plasma iron, the transfer of iron from enterocytes to the blood is reduced. In healthy subjects, the intestinal lining cells can store iron as ferritin (in which case the iron leaves the body when the cell dies and is sloughed off into feces), or the cell can move it into the blood using a protein transporter and carry it as transferrin to the rest of the body. In the bottom figure, iron overload results in more iron converted to ferritin and less converted to transferrin. The rate of absorption depends on both the region of the intestinal tract and the luminal osmolality. Because H O absorption is determined by the osmolality difference of the lumen and the blood, H O can2 2 move both ways in the intestinal tract (i. The2 water of a hypertonic meal is therefore absorbed mainly in the ileum and colon. These two communities are not the same and the genera of microbes living in the mucosa vary from those residing in the lumen. It is well established that the species composition and relative abundance of the gut microbiota are impacted by the diet, lifestyle, and overall health of an individual. Humans, like many other animals, have developed a commensalistic relationship with the gut microbiota. Over time, this relationship has evolved to become a mutualistic and interdependent one, in which the physiological activity of the microbiota has a significant impact on the host and the activity of the host impacts the genera comprising the microbiota. In support of life, gut microbial metabolism supplies the host with short- chain fatty acids, essential vitamins (i. The interactions do not end with digestion as microbial chemical signals influence other systems such as the activity of the host’s immune cells and immunologic homeostasis. In a normal, healthy individual, the interactions between the host and microbiota are primarily beneficial. However, dysbiosis can lead to, or be a contributing factor in, a number of maladies including inflammatory bowel disease (e. Clues to the development of the intestinal microbiota have emerged from many different studies. It has long been held that fetuses develop in a sterile environment within the amniotic sac. However, recent studies have shown that certain bacteria are able to cross the placental barrier. When investigators orally administered a genetically labeled species of bacteria to pregnant mice, they noted the appearance of the bacteria in both the amniotic fluid and the meconium of the pups. Others have shown that the oral microbiota is also capable of reaching, and becoming established at, the level of the placenta. Regardless, as indicated by microbial analysis of meconium, infants are born with relatively few microbes colonizing the intestinal lumen. All indications are that the major microbial colonization of the gut occurs following birth. These colonizers will generally reflect the microbial diversity present in the environment to which the infant is first exposed. For example, a vaginal birth versus one that occurs by cesarean section exposes the infant to very different microbes. Microbial recovery back to homeostasis after antibiotic treatment may take up to several months. Given the many factors that have an impact on the microbial community, there is a wide range of potential microbiota that can ultimately colonize an infant’s gut. Immediately after birth, the environment in a newborn’s gut is favorable for supporting the growth of facultative anaerobic microbes. Later, the environment favors growth of anaerobes, particularly in the distal regions of the gut with aerobes favoring the more proximal regions. By 5 years of age, the child’s gut microbial community has changed to be similar to the adult gut. The health of the host and the composition of the gut microbiota are intimately linked through the interactions that occur between the gut microbiome and the host’s innate and adaptive immune systems. These interactions have a large impact on the development of the immune system early in life and on the possibility of the host developing certain diseases in later life. Examples include local inflammatory responses in the gut (mentioned previously) and systemic autoimmune disorders such as rheumatoid arthritis, multiple sclerosis, and type 1 diabetes. Beyond the immune system, the intestinal microbiota is felt to play a role in systemic events outside the digestive tract (e. Secreted antimicrobial proteins and IgA play a role in maintaining the effectiveness of that barrier. Microbes have been implicated in other interactions that occur between the body systems. Such interactions generally result in a healthy individual with a normal body mass index.