School of the Museum of Fine Arts, Boston. V. Tizgar, MD: "Order Lithium online no RX - Best Lithium OTC".
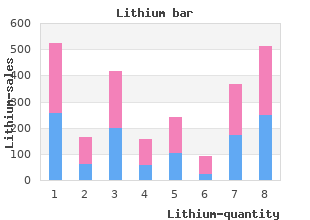
These hormones play an important role in regulating metabolic activities of the body buy 150 mg lithium fast delivery symptoms 4dp5dt, particularly glucose homeostasis generic 300mg lithium amex symptoms lyme disease. A relative or absolute lack of insulin order 150 mg lithium otc medications vs grapefruit, as seen in diabetes mellitus generic 300mg lithium with amex medications blood donation, can cause serious hyperglycemia. Left untreated, retinopathy, nephropathy, neuropathy, and cardiovascular complications may result. Administration of insulin preparations or other glucose-lowering agents (ure 24. Diabetes Mellitus the incidence of diabetes is growing rapidly in the United States and worldwide. Rather, it is a heterogeneous group of syndromes characterized by elevated blood glucose attributed to a relative or absolute deficiency of insulin. Gestational diabetes is defined as carbohydrate intolerance with onset or first recognition during pregnancy. Type 1 diabetes Type 1 diabetes most commonly afflicts children, adolescents, or young adults, but some latent forms occur later in life. The disease is characterized by an absolute deficiency of insulin due to destruction of β cells. Without functional β cells, the pancreas fails to respond to glucose, and a person with type 1 diabetes shows classic symptoms of insulin deficiency (polydipsia, polyphagia, polyuria, and weight loss). Cause Loss of β-cell function in type 1 diabetes results from autoimmune-mediated processes that may be triggered by viruses or other environmental toxins. In patients without diabetes, constant β-cell secretion maintains low basal levels of circulating insulin. A burst of insulin secretion occurs within 2 minutes after ingesting a meal, in response to transient increases in circulating glucose and amino acids. This lasts for up to 15 minutes, followed by the postprandial secretion of insulin. However, without functional β cells, those with type 1 diabetes can neither maintain basal secretion of insulin nor respond to variations in circulating glucose (ure 24. Treatment A person with type 1 diabetes must rely on exogenous insulin to control hyperglycemia, avoid ketoacidosis, and maintain acceptable levels of glycosylated hemoglobin (HbA1c). The rate of formation of HbA1c is proportional to the average blood glucose concentration over the previous 3 months. The use of home blood glucose monitors facilitates frequent self-monitoring and treatment with insulin. Type 2 diabetes is influenced by genetic factors, aging, obesity, and peripheral insulin resistance, rather than autoimmune processes. The metabolic alterations are generally milder than those observed with type 1 diabetes (for example, patients with type 2 diabetes typically are not ketotic), but the long-term clinical consequences are similar. Cause Type 2 diabetes is characterized by a lack of sensitivity of target organs to insulin (ure 24. In type 2 diabetes, the pancreas retains some β-cell function, but insulin secretion is insufficient to maintain glucose homeostasis (ure 24. In contrast to patients with type 1 diabetes, those with type 2 diabetes are often obese. Obesity contributes to insulin resistance, which is considered the major underlying defect of type 2 diabetes. Treatment the goal in treating type 2 diabetes is to maintain blood glucose within normal limits and to prevent the development of long-term complications. Weight reduction, exercise, and dietary modification decrease insulin resistance and correct hyperglycemia in some patients with type 2 diabetes. However, most patients require pharmacologic intervention with oral glucose-lowering agents. As the disease progresses, β-cell function declines, and insulin therapy is often needed to achieve satisfactory glucose levels (ure 24. It is synthesized as a precursor (proinsulin) that undergoes proteolytic cleavage to form insulin and C-peptide, both of which are secreted by the β cells of the pancreas. Secretion is most often triggered by increased blood glucose, which is taken up by the glucose transporter into the β cells of the pancreas. Mechanism of action Exogenous insulin is administered to replace absent insulin secretion in type 1 diabetes or to supplement insufficient insulin secretion in type 2 diabetes. Modification of the amino acid sequence of human insulin produces insulins with different pharmacokinetic properties. Dose, injection site, blood supply, temperature, and physical activity can also affect the onset and duration of various insulin preparations. Because insulin is a polypeptide, it is degraded in the gastrointestinal tract if taken orally. Therefore, it is generally administered by subcutaneous injection, although an inhaled insulin formulation is also available. This method of administration may be more convenient for some patients, eliminating multiple daily injections of insulin. In addition, it allows the patient to deliver a bolus of insulin to cover mealtime carbohydrate intake and compensate for high blood glucose. Adverse effects Hypoglycemia is the most serious and common adverse reaction to insulin (ure 24. Other adverse effects include weight gain, local injection site reactions, and lipodystrophy. Due to the potential for bronchospasm with inhaled insulin, patients with asthma, chronic obstructive pulmonary disease, and smokers should not use this formulation. Insulin Preparations and Treatment Insulin preparations are classified as rapid-, short-, intermediate-, or long-acting. It is important that clinicians exercise caution when adjusting insulin treatment, paying strict attention to the dose and type of insulin. Modification of the amino acid sequence of regular insulin produces analogs that are rapid-acting insulins. This modification results in more rapid absorption, a quicker onset, and a shorter duration of action after subcutaneous injection. Peak levels of insulin lispro are seen at 30 to 90 minutes, as compared with 50 to 120 minutes for regular insulin. Insulin aspart and insulin glulisine have pharmacokinetic and pharmacodynamic properties similar to those of insulin lispro. This dry powder formulation is inhaled and absorbed through pulmonary tissue, with peak levels achieved within 45 to 60 minutes. Rapid- or short-acting insulins are administered to mimic the prandial (mealtime) release of insulins and to control postprandial glucose. They may also be used in cases where swift correction of elevated glucose is needed. Rapid- and short-acting insulins are usually used in conjunction with a longer-acting basal insulin that provides control of fasting glucose.
Diseases
- Acute myeloblastic leukemia type 6
- MPS III-B
- Benign essential tremor syndrome
- Hermaphroditism
- Faye Petersen Ward Carey syndrome
- Hoyeraal Hreidarsson syndrome
- Erdheim Chester disease
Oritavancin and dalbavancin buy lithium 300mg visa medicine used to treat bv, like other lipoglycopeptides cheap lithium 300mg with visa treatment advocacy center, exert concentration-dependent bactericidal activity by disruption of bacterial membrane integrity purchase 300 mg lithium amex medications via peg tube, leading to cell death discount 300mg lithium fast delivery treatments yeast infections pregnant. Although orally administered metronidazole is absorbed nearly completely, critically ill patients with infections other than C. Metronidazole is metabolized by the liver; no dose adjustment is required in patients with renal insufficiency, but dosages must be reduced in individuals with severe hepatic insufficiency. Reported serious adverse events include neutropenia, pancreatitis, peripheral neuropathy, and hepatitis. Metronidazole is active in vitro against anaerobic Gram-negative bacilli and is probably the most potent agent for treatment of infections caused by B. Metronidazole must be used in conjunction with an agent active against aerobic organisms in the treatment of intra-abdominal, intrapelvic, and pulmonary infections where aerobic organisms can be expected to be concurrent pathogens. It has been used with great success in the treatment of anaerobic infections of the head, neck, and lungs/pleural space. The use of clindamycin in addition to penicillin is recommended in the treatment of necrotizing fasciitis due to β-hemolytic Streptococcus spp because of its apparent activity against organisms that are present in very high inoculum [32]. Because clindamycin is metabolized by the liver and excreted in inactive form in bile, no adjustment in dosage is required in patients with renal insufficiency. The most common use of macrolides is to treat primary atypical pneumonia due to Mycoplasma pneumoniae, Chlamydophilia pneumoniae, or Legionella spp; pharyngitis due to S. Erythromycin is the oldest agent in current use in this class, and now is used rarely, with azithromycin or Clarithromycin the preferred agents. In addition to sharing the microbiologic spectrum of activity of erythromycin, azithromycin is more active against C. Clarithromycin shares the antimicrobial spectrum of erythromycin but is more active against Gram- positive cocci. Both agents have activity against Mycobacterium avium- intracellulare and Mycobacterium chelonae and are used prophylactically and therapeutically for disseminated M. Second-Generation Oxazolidinones Tedizolid is approved for treatment of bacterial skin and skin structure infection with susceptible isolates of Gram-positive microorganisms including methicillin-sensitive and methicillin-resistant S. Quinupristin/Dalfopristin Quinupristin/dalfopristin is a combination of two streptogramin antibiotics used to treat infections due to vancomycin-resistant E. Daptomycin Daptomycin, a cyclic lipopeptide antimicrobial agent with rapid, concentration-dependent bactericidal activity against aerobic and facultative Gram-positive microorganisms, is active against a range of Gram-positive bacteria, including many multidrug-resistant isolates. A dose of 6-8 mg per kg every 24 hours is recommended for bacteremia and right-sided endocarditis caused by susceptible strains of S. In the lung, daptomycin is bound to surfactant, and thus it is not clinically effective for treatment of pneumonia [40]. The drug is excreted primarily via the kidney, with low potential for interference with hepatically metabolized drugs. If the creatinine clearance is less than 30 mL per minute, the dosage interval should be extended to 48 hours. Reported adverse effects include diarrhea, vomiting, sickle-cell crisis, hypersensitivity reactions, dermatitis, myalgias, and creatinine kinase elevations [41,42]. Tigecycline Tigecycline, a minocycline derivative, is the first antibiotic in the glycylcycline class [43]. The most common treatment adverse effects are nausea and vomiting which occur generally during the first 2 days of therapy. Newer antifungals of the triazole class (fluconazole, itraconazole, voriconazole, and posaconazole) and echinocandin class (caspofungin, micafungin, and anidulafungin) have become available for the treatment of systemic mycoses. However, amphotericin B remains important for empiric initial therapy for life-threatening fungal infections when the infecting organism is not yet identified or is resistant to triazoles. Amphotericin B Amphotericin B is a polyene antibiotic, insoluble in water, and solubilized by the addition of sodium deoxycholate, forming a colloidal dispersion. Its mechanism of action is due to its binding to ergosterol, a sterol present in the cell membrane of susceptible fungi, resulting in altered membrane permeability and causing leakage of cell components and resultant cell death. Either amphotericin B deoxycholate or one of the liposomal preparations is the initial drug of choice for empiric therapy of life-threatening, invasive, or systemic fungal infections including mucormycosis, cryptococcosis, histoplasmosis, and coccidioidomycosis and is effective for blastomycosis and extracutaneous sporotrichosis. Although Candida albicans generally is susceptible to amphotericin B, non-albicans species of Candida often are less susceptible, and fluconazole or an echinocandin is the drug of choice once the infecting species is identified and susceptibility is known. Amphotericin B preparations have variable activity against Aspergillus spp, Zygomycetes spp, Scedosporium boydii, Fusarium spp, and dematiaceous fungi. The combination of amphotericin B plus flucytosine is synergistic against Candida spp and Cryptococcus neoformans and is used to treat meningitis due to these fungi. The metabolism of amphotericin B is obscure, but renal and hepatic insufficiency has little effect on serum levels of the drug and hemodialysis does not affect serum levels. Daily and total doses are adjusted according to the fungal species, sites, and extent of infection and the individual tolerance of the patient. For patients who are critically ill with apparently rapidly progressive fungal disease, the full daily dose of 0. For patients who exhibit poor tolerance with the test dose or subsequent increased doses, amphotericin B dosing can be increased in a gradual fashion, with increase in the dosage by 5 to 10 mg per day until the final daily dose is reached. The usual duration of amphotericin B therapy for systemic mycoses is 4 to 12 weeks, to a total dose of 1 to 2 g. Nephrotoxicity occurs frequently with amphotericin B deoxycholate therapy, and thus patients with renal insufficiency or administration of other nephrotoxic agents should be given one of the liposomal preparations. Potassium levels should be monitored closely and supplementation with potassium begun as soon as serum potassium decreases toward the low end of normal range. Mild anemia occurs commonly during amphotericin B therapy, but thrombocytopenia, leukopenia, and severe hepatitis are rare. Alternative lipid preparations of amphotericin B have become available in an attempt to decrease renal toxicity [46]. The lipid formulations are more expensive than amphotericin B deoxycholate but are advantageous in patients with, or at risk of, renal insufficiency, those on other nephrotoxic medications, or those whose renal function worsens during treatment with amphotericin B. The ability to deliver a higher dose with the lipid complex than with amphotericin B alone has resulted in reports of patients responding to the lipid formulation at high dose (5 to 10 mg per kg) when traditional therapy with amphotericin B had been ineffective. Flucytosine Flucytosine is an orally administered pyrimidine analog with a narrow spectrum of action, generally used in combination with an amphotericin preparation for therapy of C. The drug is cleared by the kidneys, with a serum t½ of 3 hours in patients with normal renal function and 85 hours in anuric patients. The usual recommended dosage in patients with normal renal function is 150 mg per kg daily in four divided doses; the interval between doses should be doubled (every 12 hours) when the creatinine clearance rate is 20 to 40 mL per minute and quadrupled (every 24 hours) when the creatinine clearance rate is 10 to 20 mL per minute. The serum level of flucytosine should be monitored, particularly in patients with renal impairment, and the dose should be adjusted to maintain a level of 50 to 100 μg per mL. Leukopenia is the most serious complication of flucytosine therapy and occurs most commonly in patients with renal insufficiency and when serum levels exceed 100 μg per mL. Fluconazole has a long (30 hours) t½; because of its renal clearance, adjustments must be made in dosing in patients with renal impairment.
Information from the patient’s clinical presentation and physical examination are also very valuable for assessing the patient’s prognosis purchase lithium 300 mg free shipping medicine 666. For example cheap 150mg lithium with mastercard symptoms for pregnancy, it is possible to use the patient’s age and vital signs at presentation to rapidly and accurately obtain a preliminary estimate of short-term survival [10] discount 300 mg lithium mastercard symptoms dust mites. Anterior infarct location generic lithium 300mg without prescription treatment ind, delays to therapy, and information regarding medical comorbidity offer additional prognostic information [11]. At the high end, a score of more than 5 identified 12% of patients with a mortality risk at least twofold higher than the mean for the population. Discriminating among the lower risk groups, nearly two-thirds of the population had risk scores of 0 to 3 with a 5. This study found that myocardial perfusion was significantly associated with mortality independent of epicardial blood flow; using these two measures together provided incremental risk prediction. Time to Reperfusion Regardless of the choice of reperfusion strategy, several common themes are evident. Patients who receive fibrinolytic therapy within 1 hour from the onset of chest pain have an approximately 50% reduction in mortality, whereas those presenting more than 12 hours after onset of symptoms derive little, if any, benefit. For each hour earlier that a patient is treated with a fibrinolytic, there is an absolute 1% decrease in mortality [23]. Although performance metrics like door-to-balloon time have catalyzed important quality improvement efforts at the institutional level after initial presentation, broader initiatives at the systemic level aimed at reducing the total ischemic time (time from initial symptom onset to perfusion) have been equally important because total ischemic time is the principal determinant of outcome. The Fibrinolytic Therapy Trialists’ overview of all the large placebo- controlled studies reported a 2. Highlights of differences in dosing, pharmacokinetics, recanalization rates, and cost between agents are shown in Table 187. Reteplase is a double-bolus agent whereas tenecteplase is administered in a single weight-adjusted bolus. Bolus administration may minimize the risk for dosing errors, decrease “door-to-needle” time, and allow for prehospital administration. In addition, as noted previously in this chapter, approximately one-third of patients with successful epicardial reperfusion have inadequate myocardial and microvascular reperfusion [17]. However, several large and recent multicenter trials have prompted a shift in guideline recommendations. Interestingly, most patients in the standard treatment arm underwent coronary angiography, but this was performed approximately 1 day later than in the transfer arm. Although only 23% of out-of-hospital cardiac arrest cases have a shockable initial rhythm, the majority of neurologically intact survivors arise from this subgroup [28]. A randomized control trial comparing targeted temperature management to 33°C versus 36°C for patients surviving out-of-hospital cardiac arrest observed no significant differences in death or poor neurologic function at 6 months (54% vs. The benefits of aspirin are comparable to those of fibrinolytic therapy, and when used together, aspirin and fibrinolytic therapy provide additive benefits [71]. Aspirin should be initiated at an oral dose of 162 to 325 mg (preferably chewed) at the time the patient is first encountered by medical personnel in the field or emergency department. Efficacy appears to be similar at all doses greater than 75 mg, whereas bleeding risk clearly increases with higher aspirin dose. Clopidogrel reduced death, reinfarction, or stroke by 9% and death alone by 7%, both of which were statistically significant [75]. Based on the results of these two trials, clopidogrel should now routinely be added to standard fibrinolytic regimens in patients younger than 75 years [27]. Prasugrel is a second-generation thienopyridine that is more rapidly acting, more potent, and associated with less response variability than clopidogrel. In addition, there were two important subgroups in whom prasugrel was associated with excess bleeding that nullified clinical benefit, including patients >75 years of age and those <60 kg [77]. This agent provides more rapid onset (and offset) of action and a more potent and predictable antiplatelet response than clopidogrel. Ventricular pauses may also be triggered by ticagrelor early after treatment initiation, but these pauses also decrease in frequency over time, are rarely symptomatic, and have not required an excess of clinical intervention. Morphine administration also appears to reduce absorption of P2Y12 inhibitors and contribute to delayed onset of action [79–81]. Cangrelor is a novel intravenous, fast-acting, and reversible P2Y12 inhibitor that may offer an alternative strategy for patients to achieve rapid P2Y12 inhibition. Given the high cost, at the present time, we generally limit cangrelor use to patients unable to take oral P2Y12 inhibitors. In a meta- analysis involving 3,266 patients enrolled in four randomized trials comparing abciximab with placebo, patients receiving abciximab had a 46% reduction in 30-day death, reinfarction, and urgent target vessel revascularization compared to those who received placebo [83]. Moreover, data are very limited in the current era of more potent and rapidly acting P2Y12 inhibitors. An issue of concern was an increased risk of stent thrombosis within the first 24 hours in the bivalirudin group. Compared with bivalirudin, heparin reduced the incidence of major adverse ischemic events in the setting of primary percutaneous coronary intervention, with no increase in bleeding complications. The availability of P2Y12 inhibitors has virtually eliminated the past reliance on warfarin for aspirin-allergic patients. It should be noted that the newer direct oral anticoagulants have not been evaluated in this clinical context, so their use cannot be recommended. An increasingly challenging scenario relates to the combination of aspirin, a P2Y12 inhibitor, and warfarin. It may be expected that risks will be even higher with combinations that include the newer and more potent antiplatelet agents such as prasugrel and ticagrelor. Surprisingly, the group randomized to withhold aspirin also had markedly lower rates of all-cause mortality than the triple therapy group (2. Ongoing research efforts continue to search for the optimal risk/benefit profile in this complex patient population. The fact that β-blockers were particularly effective in reducing sudden death and reducing mortality among patients with complex ventricular ectopy at baseline suggests that β-blockers exert much of their beneficial effect by reducing the frequency and severity of arrhythmias [96]. Post hoc analyses indicate that this increased risk was predominantly among patients with indicators of or risk factors for hemodynamic compromise. Parenteral β-blockers should be used only if there is a clear indication such as ongoing chest pain or an atrial tachyarrhythmia with normal or elevated blood pressure [27]. Aldosterone antagonists should be avoided in patients with hyperkalemia or significant renal dysfunction (Table 187. Nitrates Nitrates dilate large coronary arteries and arterioles, peripheral veins, and to a lesser extent, peripheral arterioles. Neither study found a significant reduction in mortality with nitrates, although the ability to detect such a difference may have been reduced because more than 50% of patients received off-protocol nitrates. Calcium Channel Blockers Calcium channel blockers block the entry of calcium into cells via voltage- sensitive calcium channels. Sustained-release preparations of nifedipine, on the other hand, can be used safely in combination with a β- blocker.
When lished in 2014 states categorically that low‐dose regi- offered this form of medication women should be mens should be used for the initiation and maintainence informed of this purchase lithium 150mg with visa symptoms 1 week before period. The latter involves ultrashort‐acting opioid remifentanil has theoretical injection of the initial dose into the intrathecal space advantages over other opioids owing to its short latency (a spinal injection) prior to placing an epidural catheter purchase 300 mg lithium otc medicine 831. However generic 150 mg lithium with amex medications used to treat fibromyalgia, respiratory depression the intrathecal dose requires one‐tenth of the amount of occurs in over 30% of women and cases of hypoxic car- local anaesthetic to be effective and provides almost diac arrest have been reported lithium 150mg on line treatment 2. It may also provide more reli- used in units where staff are experienced in and regularly able analgesia throughout labour and the use of com- care for women with this type of analgesia [1]. There is growing evidence that the effects of regional Regional analgesia analgesia on the progress and outcome of labour are dose related. Systematic review of randomized con- There is no question that neuraxial blockade (epidural or trolled trials comparing regional and non‐regional (opi- intrathecal) provides the most effective form of pain oid) analgesia shows that regional analgesia does not relief in labour, and very few women cannot benefit from increase the overall risk of caesarean delivery but may be this form of analgesia (Table 30. Regional analgesia prolongs the second stage of labour (by approximately 15min) and Table 30. Evidence from Absolute randomized controlled studies suggests that low‐dose Maternal refusal neuraxial regimens are associated with fewer instrumen- Lack of personnel/facilities Pre‐existing coagulopathy tal deliveries compared with conventional epidural anal- Local infection at insertion site gesia [14]. Concerns about impaired maternal effort in Raised intracranial pressure (risk of coning) the second stage of labour have resulted in the wide- Drug allergy spread habit of discontinuing regional analgesia in late Relative labour [15]. However, a recent review concludes that in Haemodynamic instability the absence of large trials the evidence suggests that all Anatomical abnormalities this achieves is poor analgesia in the second stage of Neurological disorders (medicolegal implications) labour [16]. Neither is there any evidence to withhold Systemic infection neuraxial analgesia from women in the latent stage of Analgesia, Anaesthesia and Resuscitation 425 Table 30. Single‐shot spinal* Epidural Combined spinal–epidural Onset of action (min) Fast (1–5) Slow (10–20) Fast (1–5) Median pain score 60–90 min 0 0–3 0 Total drugs dose Low High Low Observable leg weakness (%)† 100 5–50 0–40 Post‐dural puncture headache (%) 1–2 0. Presenting part of fetus engaged and well applied to cervix Ambulation in labour has not been shown to signifi- Minimal or no motor and proprioceptive block cantly affect the mode of delivery, However, mobility No postural hypotension may decrease analgesic requirements and avoids the Continuous fetal monitoring (cardiotocography) when indicated risks associated with prolonged recumbency. Mobilizing Suitable conditions with regional anaesthesia has been shown to be safe and Good epidural catheter fixation is viewed positively by women who undertake it [17]. To Attending midwife permit safe ambulation, all delivery unit staff must be Disconnection of intravenous line (bung inserted) appropriately trained and certain conditions must be No shoes met (Table 30. Motor and proprioceptive block must Safe, even floor without cables, steps or mats be excluded. Studies have demonstarated that women themselves can reliably tell if they can ambulate safely [18]. Results are currently awaited from a study compar- shown to be effective) that can be rapidly replenished ing upright and recumbent positions in the second stage (e. Obesity per se may become a major indication for this type of analgesia, Summary box 30. Difficulties in siting neuraxial Reduced doses of local anaesthetics decrease the inci- blocks make its early use advisable. Royal College of Anaesthetists found that serious com- plications associated with death or permenent sequelae were rarer than previously estimated [19]. Although There are several obstetric and medical indications for approximately 50% of all blocks performed are in the neuraxial block in labour in addition to the need for pain obstetric population, the incidence in this population relief (Table 30. Cases considered at high risk of was low compared with other patient populations possi- requiring intervention for delivery benefit from an bly due to the general level of good health of obstetric indwelling epidural catheter (which has been tested and patients. Anaesthesia for caesarean section Pain relief the increased use of regional anaesthesia for caesarean Avoid the deleterious effects of pain (maternal exhaustion, section has contributed to the fall in anaesthetic‐related raised catecholamines, maternal and fetal acidosis) maternal mortality. The great majority of anaesthetic‐ Reduce premature urge to push related maternal deaths are due to general anaesthesia, Anaesthesia for manual removal of placenta particularly in the emergency situation. General anaes- Reduce need for emergency general anaesthesia thesia is particularly hazardous in obstetrics because of Multiple pregnancy (rapid anaesthesia for delivery of after‐ changes associated with pregnancy that increase the risk coming twin if required) of difficult or failed intubation, of hypoxia and of aspira- Breech tion. General anaesthesia is frequently reserved for the Suspected cephalopelvic disproportion/macrosomia extremely urgent section when the anaesthetist, who may not have previously met the patient, has very little? Obesity anaesthesia is used less and less in obstetrics, skills will Improve uteroplacental flow/fetal condition dwindle increasing the risks of this type of obstetric Pre‐eclampsia anaesthesia. However, in the most urgent cases, up Improve maternal condition to a 15% rate of conversion to general anaesthesia may be expected. The four‐grade classification of urgency of caesarean sec- Reduces circulating catecholamines (especially maternal fixed cardiac output states) tion, endorsed by the Royal College of Obstetricians and Gynaecologists and the Royal College of Anaesthetists and Decreases urge to push (Valsalva manoeuvre) in second stage used in the National Sentinel Audit of caesarean sections, should be universally adopted to improve communication Table 30. Prior to sched- uled surgery, regardless of the type of anaesthetic planned, Complication Incidence patients should be fasted (6 hours for solids, 2 hours for clear fluids) and given premedication (oral ranitidine and Cardiovascular collapse Very rare metoclopramide). Labouring women at risk of caesarean High total spinal (relative/absolute overdose section should be limited to sips of water and given oral ran- of local anaesthetic) itidine 150mg 8‐hourly throughout labour. Intravenous Local anaesthetic toxicity (inadvertent ranitidine 50mg may be given within 30min of induction intravenous administration) whereas sodium citrate, which is only effective for Infection (epidural abscess) 1 in 145 000 15–30min, should be given immediately before induction Meningitis of general anaesthesia. In the emergency situation, intrau- Epidural haematoma 1 in 168 000 terine resuscitation of the fetus (Table 30. Oxygen Trauma (direct damage to spinal cord/nerve root damage) therapy in the presence of profound fetal distress is still rec- ommended, although the evidence is not compelling [24]. Incidence of Relieve aortocaval compression: left lateral position ≥15° tilt, epidural hematoma, infection, and neurologic injury in obstetric patients uterine displacement with epidural analgesia/anesthesia. Ensure effective analgesia: top up epidural (decreases maternal catecholamine levels and improves uteroplacental blood flow) Rapid intravenous infusion (transiently decreases uterine permenent harm in the obstetric population resulting activity) from neuraxial blockade was between 0. Analgesia, Anaesthesia and Resuscitation 427 Regional anaesthesia is recommended in severe pre‐ hypoxia. Local anaesthetic toxicity and magnesium over- eclampsia as haemodynamic stability is better main- dose also occur in this population. Lack of knowledge of tained than in the normotensive patient and because the resuscitation (both basic and advanced) among healthcare risks of general anaesthesia are further increased in professionals caring for maternity patients has repeatedly pre‐eclampsia. In consecutive reports on maternal as an absolute indication for general anaesthesia. One of the ‘top ten’ mother to be awake for delivery, after which general recommendations of the 2003–2005 report was that ‘All anaesthesia can be induced for caesarean hysterectomy staff must undertake regular, written, and audited training or other complicated surgery. Similarly for fetal surgery, for the improvement of basic, immediate and advanced or other surgery during pregnancy, combined general life support skills’. A growing number of courses are avail- anaesthesia and regional blockade is frequently used. Training should be supplemented by regular team the combined spinal–epidural technique allows effec- practice of cardiac arrest drills to ensure appropriate care tive anaesthesia to be prolonged as long as required and is delivered [28]. Cardiopulmonary resus- citation is both more difficult to perform and less effective in the obstetric patient. The Royal College of Anaesthetists recommends ine displacement or pelvic tilt is required. Because of the that more than 85% of emergency and more than 95% of importance of uninterrupted cardiac compressions and elective caesarean sections should be performed under because effective cardiac compression becomes progres- regional anaesthesia. Hypoxia develops more quickly due to increased oxygen require- ments and decreased oxygen reserves. Artificial ventila- Cardiopulmonary resuscitation tion becomes more difficult due to enlarged breasts and and critical care decreased lung compliance resulting from the enlarging uterus.
Generic lithium 300 mg amex. Abdominal pain and Dehydration (Medical Symptom).