North Carolina School of the Arts. C. Hamil, MD: "Purchase cheap Clonidine - Proven Clonidine OTC".
The presence of a vaginal discharge should suggest candidiasis clonidine 0.1mg lowest price hypertension specialist doctor, trichomoniasis vaginitis clonidine 0.1 mg on line prehypertension prevention, and bacterial vaginitis safe clonidine 0.1 mg blood pressure charts readings. The presence of a rash would suggest eczema order clonidine 0.1 mg with amex blood pressure medication names starting with t, herpes simplex, folliculitis, scabies, and tinea infections. The presence of a lesion in the vulva or vagina would suggest kraurosis vulvae, leukoplakia or vulval carcinoma, condylomata lata, and condylomata acuminata. Pseudoptosis occurs when there is inflammation of the eyelid, cornea, or other ocular structures. Periorbital edema, conjunctivitis, and trachoma are among the many disorders to consider. Intermittent ptosis would suggest myasthenia gravis, ophthalmoplegic migraine, and transient ischemic attacks. The presence of partial ptosis would suggest Horner’s syndrome, especially if there is a constricted pupil. However, myotonic dystrophy, myasthenia gravis, and progressive muscular atrophy are just three of the disorders that may present with partial ptosis. The presence of a dilated pupil, especially with a unilateral ptosis, suggests a ruptured cerebral aneurysm. However, if the dilated pupil is associated with many other neurologic signs, then there are many other conditions to consider. The presence of a constricted pupil with unilateral complete ptosis would suggest diabetic neuropathy. However, if there is bilateral complete ptosis, chronic progressive external ophthalmoplegia and myasthenia gravis should be considered. The presence of other cranial nerve signs should suggest cavernous sinus thrombosis, cerebral aneurysm, tuberculous meningitis, syphilitic meningitis, Wernicke’s encephalopathy, diphtheria, and subdural hematoma. The presence of hyperactive reflexes would suggest syringomyelia, platybasia, brain stem tumors, vertebral basilar occlusion or insufficiency, multiple sclerosis, epidemic encephalitis, and general paresis. The presence of hypoactive reflexes would suggest myotonic dystrophy, tabes dorsalis, and progressive muscular atrophy. If a neurologic 522 disease is suspected, a neurologist should be consulted, especially if the onset is acute. If myasthenia gravis is suspected, a Tensilon test and acetylcholine receptor antibody titer can be done. If encephalitis, meningitis, central nervous system lues, or multiple sclerosis are suspected, a spinal tap may be useful. If muscular dystrophy is suspected, a 24-hour urine collection for creatinine and creatine and a muscle biopsy may be done. Cerebral angiography will be necessary to diagnose most cerebral aneurysms and cerebral vascular disease, including transient ischemic attacks. Mercury, iodides, and mouthwash are some of the substances that may cause ptyalism. Peritonsillar abscess, carious tooth, ulcerating tumor, herpes simplex, aphthous stomatitis, and ill- fitting dental plates are all conditions that may cause ptyalism. The presence of abnormalities on the neurologic examination should suggest pseudobulbar palsy, bulbar palsy, Parkinsonism, dementia, idiocy, rabies, and facial palsies. A neurologist is in a better position to determine which of these studies is appropriate in any given case. However, frequently, there is simply a benign or malignant tumor over a large artery that gives the false impression that the mass is an aneurysm when it is not. In the abdomen, a normal abdominal aorta may be mistaken for an aortic aneurysm, especially in thin patients. In the neck, normal carotid, brachial, or innominate arteries may pulsate vigorously when there is aortic regurgitation. Eggshell cracking along with the pulsation in a mass should suggest an osteosarcoma. A pulsating mass in the right upper quadrant is most likely the enlarged liver because of tricuspid regurgitation or stenosis. All other cases of pulsatile masses suggesting an aneurysm should receive angiography of the artery or arteries supplying the area. A rapid rate would suggest supraventricular tachycardia, ventricular tachycardia, atrial flutter, and fibrillation. A rapid regular rate would suggest supraventricular tachycardia or ventricular tachycardia, whereas a rapid irregular rate would suggest atrial flutter or fibrillation. A slow irregular rhythm would suggest Wenckebach phenomena or sick sinus syndrome. Newer technology includes using a continuous-loop event recorder to allow monitoring for 2 weeks at a time. Also, angiography and catheterization studies should be considered in difficult cases. Acute reduction of the pulse of an extremity may be because of an arterial embolism, dissecting aneurysm, or fracture of the limb. The upper extremities are involved selectively in the subclavian steal syndrome, Takayasu’s disease, a few cases of coarctation of the aorta, congenital anomalies, thoracic outlet syndrome, aneurysm of the arch of the aorta, and supravalvular aortic stenosis. The presence of transient ischemic attacks should suggest subclavian steal syndrome and Takayasu’s disease. Involvement of the lower extremities only would suggest peripheral arteriosclerosis, Buerger’s disease, arteriovenous fistula, and Leriche’s syndrome. Involvement of both the upper and lower extremities would suggest coarctation of the aorta and dissecting aneurysm. With a history of trauma, plain films of the involved extremity are essential to rule out fracture. The presence of a dilated pupil should suggest oculomotor nerve palsy such as may be because of a ruptured aneurysm or intracranial hematoma. However, if the pupil reacts to light and accommodation, a local condition such as iritis, glaucoma, anisocoria, or irritation of the cervical sympathetic nerves must be considered. If the pupil reacts to accommodation but not to light, then central nervous system syphilis must be suspected. If there is no reaction to light or accommodation, blindness must be considered because of optic nerve lesions. This finding would suggest a local condition, such as iritis, glaucoma, anisocoria, or irritation of the cervical sympathetic nerves. If there is no ptosis with the constricted pupil, a brain stem lesion, such as syringomyelia, tumor, abscess, or encephalitis must be considered. If there is fever or a history of trauma with dilated or constricted pupils or other pupillary abnormalities, a neurologist or neurosurgeon should be consulted immediately before ordering expensive diagnostic tests. A spinal tap will help diagnose central nervous system lues or multiple sclerosis. The presence of a petechial rash suggests either a thrombocytopenic purpura, which may be idiopathic or secondary to leukemia, aplastic anemia, collagen disease, or drugs. In addition, petechiae may suggest platelet dysfunction, in which case the platelet count will be normal, or vasculitis, such as from collagen diseases, hereditary telangiectasia, scurvy, or drugs. The presence of a normal platelet count would suggest either thrombocytopathy or vasculitis.
The gun is now activated which repairs the cut mucosa and submucosa by stapling the edges together discount clonidine 0.1 mg amex blood pressure under 80. This technique is less painful and less traumatic than conventional haemorrhoidectomy generic 0.1mg clonidine visa arrhythmia young. Large haemorrhoids particularly those which are prolapsing are suitable for elastic band ligation cheap clonidine 0.1mg on-line heart attack right arm, but it is a painful method buy clonidine 0.1 mg lowest price blood pressure specialist. Cryotherapy is also effective for the same group of patients, but is more expensive and causes considerable discharge and loss of work than elastic band ligation. Lord’s dilatation has a place in the treatment of acute thrombosed prolapsed piles, but find little place for routine management of haemorrhoids. For large third degree and fourth degree piles particularly with skin tags and external piles haemorrhoidectomy remains the only form of treatment which can guarantee lasting results. Fissures occur most commonly in the midline posteriorly, the least protected part of the anal canal. In males fissures usually occur in the midline posteriorly (90%) and much less commonly anteriorly (10%). In females fissures on the midline posteriorly are slightly commoner than anteriorly (60 : 40). The relative frequency of the anterior fissures in the females may be explained by the trauma caused by the foetal head on the anterior wall of the anal canal during delivery. Spasm of the internal sphincter has also been incriminated to cause fissure- in-ano. When too much skin has been removed during operation for haemorrhoids, anal stenosis may result in which anal fissure may develop when hard motion passes through such stricture. These are : (i) Ulcerative colitis, (ii) Crohn’s disease, (iii) Syphilis and (iv) Tuberculosis. So whole of the anal fissure lies in the sensitive skin of the anal canal and that is why pain is the most prominent symptom. Chronic fissure-in-ano is a deep canoe-shaped ulcer with thick oedematous margins. At the lower end of the ulcer there is a skin tag known as ‘sentinel pile’ (sentinel because it guards the anal fissure). Crohn’s disease, ulcerative colitis, tuberculosis and syphilis, so during operation biopsy must be taken from a chronic fissure to exclude secondary cause mentioned above. Constipated hard stool while passes through the anal canal in patients where there is spasm of internal sphincter and hypertrophied anal papilla an acute tear of the anal canal will occur. If the acute fissure fails to heal, it will gradually develop into a deep undermined ulcer. A typical chronic fissure-in-ano will have in its upper end a hypertrophied anal papilla. At its lower end a tag of hypertrophic skin, which is called a sentinel pile and canoe-shaped ulcer in between the upper and lower ends. Pain starting with and following defaecation (usually following an hour or more) has been variously described as sharp, biting, burning etc. Haemorrhoids may be associated with fissure-in ano and it must be remembered that uncomplicated haemorrhoid in first and second degrees are usually without pain. After the pain goes off the sufferer remains comfortable till the next action of bowel. The bleeding of anal fissure is variable, but usually occurs as streaks on the outside of the stool or spots noted on toilet tissue (cf. If the margins of the anus are gently separated, the lower end of the anal fissure may be inspected. When the patient does not allow digital examination, a surface anaesthetic such as 5% xylocaine ointment may be applied on the anus and digital examination may be tried after 5 minutes. In more difficult cases, digital examination and proctoscopy may not be possible without general anaesthesia. But in chronic fissure, the characteristic crater of the vertical fissure may be felt. The pain may be unbearable and possibly due to segmental cramp of the pubococcygeus muscle. It is said to be seen more commonly in patients who are in undue stress or anxiety. A more chronic form of the disease has been termed the ‘levator syndrome’ and may be associated with severe constipation. A few enthutiastic surgeons have tried to sever the puborectalis muscle, but this should not be done, as it causes incontinence. Conservative treatment includes (a) oral pain medication, which may be taken before any anticipated bowel movement, (b) Stool softner may be used to make the stool soft enough to be passed without anal spasm. Weak bulk laxative or cathartics is best in this condition, (c) Nitric oxide is a neurotransmitter which induces relaxation of the internal sphincter. Glyceryl trinitrate is a nitric acid donor and is applied as an ointment to the anal canal to produce the relaxation of the internal sphincter. Moreover glyceryl trinitrate improves blood flow to the area which further helps in healing of the fissure. But glyceryl trinitrate has a few side effects of which severe headache is of main concern. This technique of using xylocaine lubricant and then dilating the anal canal with dilator should be practiced twice a day for a month. By this time the anal fissure may be healed, (f) Injection of long acting anaesthetic solutions promotes little relief and has significant complications. Under general anaesthesia and the patient in lithotomy position the index and the middle fingers of each hand are inserted simultaneously into the anus and pulled apart to give maximal anal dilatation. Any constricted bands should be well stretched and the fibrosis around the fissure should be ironed out. The patient can go home the same day, but should be warned that there may be some faecal incontinent for 10 days. When the chronic fissure is with excessive fibrosis and skin tag, there is every chance that anal dilatation will be a failure. The fibres of the internal sphincter will be seen running transversely in its floor. It must be remembered that only superficial fibres of the internal sphincters are divided and not the entire thickness of the internal sphincter. Postoperative treatment includes liquid diet for 2 days and the bowel is moved on 3rd day. After moving bowel a daily hip bath and passage of an anal dilator are required till the wound is absolutely healed. The only disadvantage of this operation is a prolonged convalescent period of 7 to 10 days and in occasional cases there may be persistent mucous discharge. Though it is said that the convalescent period is less in this operation, yet this operation is handicapped in the sense that excision of the ulcer or biopsy cannot be performed in one go.

It is not strictly necessary to mobilize the esophagus fully both anteriorly and posteriorly if both M y o t o m y the narrowed segment and the dilated segment above it are easily visualized once the hiatus has been cleared purchase clonidine 0.1mg with visa blood pressure chart india. Many sur- Begin the myotomy at a convenient location on the midpor- tion of the thickened distal esophagus (Fig clonidine 0.1 mg otc blood pressure quiz. Curved scissors attached to electrocautery are useful for splitting generic clonidine 0.1 mg online arrhythmia life threatening, elevating buy clonidine 0.1mg with amex blood pressure during exercise, lightly cauterizing, and cutting parallel to the lon- gitudinal muscle fibers. Use atraumatic graspers to elevate and pull down on the longitudinal muscle to improve expo- sure (Fig. Release the tension on the Penrose drain (if one was placed) to avoid pushing the walls of the esophagus together, which would increase the proba- bility of injury to the epithelial tube. Sequentially elevate the circular muscle fibers on the blade of the scissors, lightly cauterize, and cut. As the esoph- ageal wall starts to open, place atraumatic graspers on the left and right cut edges of the muscular tube and pull gently apart and toward the patient’s feet. Release all instruments from the epithelial tube with the blade of the scissors and cutting the esophagus. The opening should avoid burning the underlying epithelial tube, and pull it down be patulous if an adequate myotomy was performed. Gastroesophageal reflux Esophageal perforation Fundoplication Further Reading Some surgeons perform a partial fundoplication at the con- clusion of the procedure. Laparoscopic Heller’s cardio- a simple way to buttress a small (repaired) perforation. We use a partial Comparison of outcomes following open and laparoscopic esoph- fundoplication selectively. Heller myotomy ver- scopic modified Heller myotomy for achalasia: efficacy and safety sus Heller myotomy with Dor fundoplication for achalasia: a pro- in 87 patients. Chassin† Indications Operative Strategy Instrumental or emetogenic esophageal perforation Visualize and thoroughly explore the region of the perfora- Postoperative leak tion. What appears to be a 1-cm perforation may prove to be three to four times that length after it is mobilized from the mediastinal pleura. Debride necrotic material around the per- Preoperative Preparation foration if suturing is anticipated. When the defect appears too large or the tissues too inflamed for suturing, it may be Confirm perforation with diagnostic studies such as chest possible to apply a roof patch consisting of a flap of muscle radiography; for suspected cervical perforations, lateral pedicle, pleura, or pericardium that is sutured over the neck films in hyperextension; computed tomography perforation. Administer nasoesophageal suction proximal to perforation of the thoracic esophagus. Operative Technique Pitfalls and Danger Points Pleural Flap Repair of Thoracic Delayed diagnosis of the perforation Esophageal Perforation Inadequate attention to pulmonary function Inadequate surgery to control continuing contamination Incision Inadequate drainage Make an incision in the left or right thoracic cavity depending Depending on sutured closure of inflamed esophagus on which side the perforation appears to present on the con- Suturing a perforated esophagus proximal to an obstruction trast esophageal radiograph. Generally, the lower half of the Inadequate pleural toilet and lung decortication esophagus is approached through a left sixth or seventh inter- costal space thoracotomy. Chassin esophagus so the esophagus can be elevated from its bed for thorough exploration. If the perforation is not immedi- ately apparent, ask the anesthesiologist to instill air or a solu- tion of methylene blue into the nasoesophageal tube and look for bubbling or the area of blue staining on the esophageal wall. Most patients have a pleural and a significant mediastinal infection with necrosis. Complete debridement of the medias- tinum and decortication of the lung with removal of both pari- etal and visceral peels are used to control infection and ensure maximal lung function. Complete expansion of the lung is the best secondary defense against breakdown of an esophageal repair and helps control any fistula that develops. Repair When operation is performed soon (8 h) after perforation, it may be possible to debride the tissues around the esophagus if marked edema and inflammation have not yet occurred; a viable tissue buttress should always be added to the repair. For suture closure, close the mucosal layer with interrupted sutures of 4-0 or 5-0 nonabsorbable synthetic suture and approximate the muscular layer with interrupted Lembert Fig. There must be sufficient good tissue to achieve an everted stapled closure without narrowing the lumen. Mobilize the edges of the effect and use Allis clamps to bring the full thickness of the esophageal wall within the jaws of a linear thick tissue stapler. If the perforation is located in the lateral aspect of the esophagus, a simple rectangular flap of pleura is ele- vated and brought over the suture line. Use many interrupted 4-0 nonabsorbable sutures to fix the pleural flap around the sutured perforation. When the perforation is not suitable for a sutured closure due to marked edema and inflammation, employ a pleural flap, an intercostal muscle flap, or some other viable buttress as a roof patch over the open defect in the esophagus. When the esophagus is too inflamed to hold sutures, it is advisable to exclude the upper esophagus from the gastroin- testinal tract by one of the methods described below to sup- plement the pleural roof patch. With an extensive defect in the esophagus or one located on the posterior surface, outline a large rectangular flap of pleura as illustrated in Fig. In the presence of mediastinitis, the pleura is thickened and easy to mobilize from the posterior thoracic wall. Insert multiple 4-0 interrupted non- absorbable sutures deep enough to catch the submucosa of Drainage the esophagus around the entire circumference of the perfo- Place the tip of a 36 F chest tube near the site of the ration as well as the entire circumference of the esophagus esophageal perforation. Suture it to the mediastinal tis- above and below the perforation, as illustrated in Fig. Bring this tube out through a 27 Operations for Esophageal Perforation and Anastomotic Leaks 261 Fig. Intercostal Muscle Flap Repair of Esophageal Perforation Another method for bringing viable tissue to the site of an esophageal perforation is to create a vascularized flap of the appropriate intercostal muscle with which to wrap the perforation of the esophagus. If the patient undergoes sur- gery within the first 8 h after a perforation, minor debride- ment and primary suturing generally remedy the situation. However, for perforations that have been leaking for a longer interval before surgery is undertaken, debridement of necrotic tissue and primary suturing may not be ade- quate; in these situations wrapping with a viable muscle flap may help achieve primary healing. In cases where the perforation is too large for suture closure, a roof patch consisting of viable intercostal muscle sutured to the Fig. Large perforations (longer than the width of the muscle preserve the intercostal vessels. Drain the attached to the muscle as it is being dissected away from the mediastinum and chest as described above. Chassin beginning 2–3 cm below the level of the mandibular angle and continuing down to the clavicle (see Fig. Retract the sternomastoid muscle and carotid sheath laterally and retract the prethyroid muscles medially, exposing the thyroid gland (see Fig. Carefully divide the areolar tissue between the thyroid gland and the carotid sheath to expose the inferior thyroid artery and the recurrent laryngeal nerve. Begin the dissection on the prevertebral fascia and free the esophagus posteriorly.
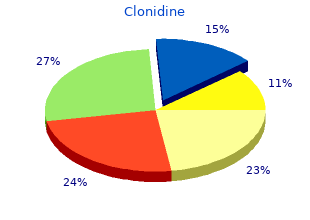
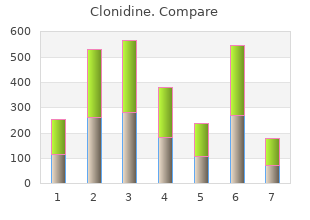
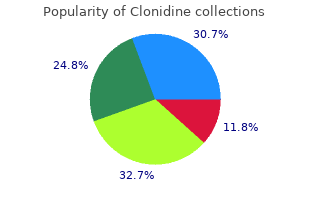
| Comparative prices of Clonidine | ||
| # | Retailer | Average price |
| 1 | Starbucks | 909 |
| 2 | Price Chopper Supermkts | 512 |
| 3 | Verizon Wireless | 524 |
| 4 | Wal-Mart | 207 |
| 5 | Burger King Holdings | 375 |
| 6 | Walgreen | 173 |
| 7 | Albertsons | 520 |
| 8 | Sherwin-Williams | 959 |