Medical College of Ohio. P. Fraser, MD: "Purchase online Atenolol cheap - Cheap Atenolol online".
The palm is then placed in a plaster of Paris cast followed by further X-ray assessment for a period of approximately 4 weeks purchase atenolol 100mg amex blood pressure diet. In many cases the carpal bones need to be stabilized with the insertion of K-wires which are subsequently removed order atenolol 100mg line heart attack age. Traumatic dislocation of the hip usually occurs Knee joint dislocation This is a relatively uncommon posteriorly purchase atenolol 50 mg fast delivery heart attack from weed. The joint usually dislocates anteriorly but it mitted through the knee to a flexed hip order atenolol 50mg mastercard blood pressure recommendations, such as a can dislocate posteriorly, medially or laterally. It of the knee joint ligaments – the medial collateral, can also occur following a fall. Associated injuries lateral collateral, anterior and posterior cruciate include acetabular fracture or fracture of the femo- ligaments – are inevitably injured and there may be ral head/shaft. Neurovascular structures are at risk, par- ticularly the common peroneal nerve and the pop- Investigation liteal artery. Clinical diagnostic indicators Investigation Clinically, the hip is flexed and shortened with internal rotation. Approximately 10 per cent of dis- The integrity of the popliteal nerve and its branches locations are associated with a sciatic nerve palsy. If there is an associated fracture, pelvic inlet severity of the associated soft tissue injuries. The dislocation is reduced by traction and manipu- lation followed by either a period of immobiliza- Management tion or an immediate or delayed direct surgical repair of the damaged structures, including the The dislocation should be reduced by traction and ligaments within the joint. Following reduction, the leg is placed in traction This rarely occurs without an associated fracture. If significant fractures are recognized, open reduction and internal fixation may be required. Therefore a detailed description of their investigation and management Patella dislocation This can be caused by a direct blow would be out of place in this introductory student’s at the side of the knee or a sudden muscular con- textbook. Plain X-rays should be taken to confirm the Be suspicious of their possible presence dislocation. The patella is manipulated back into If your suspicions are confirmed, refer urgently place and the knee joint immobilized in plaster or to a specialist multidisciplinary centre. Any non- A tissue biopsy is best performed in the special- mechanical unexplained skeletal pain, especially at ist referral centre, as inappropriate sampling can night, unrelieved by rest or anti-inflammatory lead to tumour spread and also potentially compro- medication should arouse suspicion. Management Further symptoms and signs of bone tumours Once the diagnosis has been confirmed, treatment are well described in our companion volume. Blood test and urine analysis Simple cysts and aneurysmal bone cysts may A full blood count with differential, biochemistry undergo curettage, bone grafting or injection. In higher grade Imaging tumours, more radical excision is necessary, often Plain X-rays of the painful bone may show a space followed by bone graft and prosthetic replacement. Amputation can be a last resort and is not Ultrasound is more valuable for soft tissue indicated until the absence of metastatic spread is lesions. An isotope bone scan may detect isolated lesions Chemotherapy may be required before and after or multiple metastases. These tests should be sufficient to confirm your Radiotherapy is suitable for some sensitive clinical suspicions and justify referral to a specialist tumours such as Ewing’s sarcoma. Corbett Most of the clinical problems that arise in the upper overlying the shoulder joint’s capsule. Its functions limb are caused by diseases in and around the limb’s include elevating the arm (supraspinatus) rotating many joints. The rotator cuff also plays an impor- pain tant role in holding the humeral head stable in the stiffness glenoid fossa of the scapula when the arm is moved. The short head of biceps arises The diseases that cause these problems affect all from the coracoid process and is outside the joint. This chapter describes the The subacromial bursa is the largest bursa investigation and management of the mechanical within the shoulder and lies between the cuff’s disturbances and diseases of the shoulder, elbow tendons and the coracoacromial arch. The coraco- and hand that give rise to the common problems acromial arch is formed by the acromion, the listed above. This bursa allows the rotator each joint in order to appreciate how mechanical cuff to glide during movement. The rotator cuff comprises the supraspinatus, Clinical diagnostic indicators infraspinatus, teres minor and subscapularis tendons, The impingement syndrome is pain in the subacro- which insert into the greater and lesser tuberosities of mial space when the humerus is elevated or inter- the humerus. This is classically described as the to the front, top and back of the head of the humerus painful arc between 60 degrees and 120 degrees, 172 The bones, joints and soft tissues of the upper limb Physiotherapy and a short course of anti- inflammatory medication are the first-line management. Injection of local anaesthetic and cortisone into the subacromial space is performed if this fails. Patients should not be subjected to numerous injections as other potentially successful treatment options are available. The under- surface of the anterolateral acromion is cleared and smoothed, the coracoacromial ligament is released and the subacromial bursa excised. The range may however, Patient satisfaction rates are reported to be vary and pain is sometimes experienced in a higher 98 per cent following this procedure. Patients present with pain at 90 degrees eleva- Tears of the rotator cuff may occur in any of the tion and also when internally rotating the shoulder tendons but the supraspinatus is most frequently in this position. The tear can be partial or complete and can formed in which local anaesthetic is injected into be caused by trauma or, more commonly, following the subacromial space. Investigation Imaging Clinical diagnostic indicators Plain X-rays may show narrowing of the acromio- The patient may be symtomless, or have pain or humeral distance together with sclerosis on the weakness, which may manifest in an inability to under-surface of the acromion (sourcil sign) raise the arm. Ultrasound scanning may demonstrate evi- Imaging dence of inflammation and of structural changes X-rays may show a reduction of the space between within the tendons and the subacromial bursa. The scan features of impingement (see above) can be used as a dynamic test to show the impinge- An ultrasound scan can demonstrate partial ment as the patient moves their arm. Corticosteroid injection into the subacromial What was the activity level of the patient before space may also be tried, but repeat injections the tear? The edges of a partial tear may be measuring inflammatory markers, should be con- excised or the tear completed and repaired. This sidered as the differential diagnosis of acute calcific can be achieved either by an arthroscopic or by an tendonitis includes septic arthritis of the gleno- open surgical technique and is generally combined humeral joint. Management In the older age group, the edges of the tear In the early phase, the arm should be rested with can be excised arthroscopically and a subacromial a short course of anti- inflammatory medication. Muscle transfer procedures using latissimus dorsi may be tried if a rotator cuff tear is massive and irreparable. If there is associated glenohumeral joint arthritis (cuff tear arthropathy) a shoulder hemiarthroplasty or shoulder joint replacement can be performed. The pain, which is caused by swelling and pressure within the ten- don, is sometimes so intense that the patient will present themselves to the Accident and Emergency Department as an emergency. The symptoms how- (A) ever, usually improve over a period of 7–10 days, with the shoulder returning to normal within a 6-week period. In chronic calcific tendonitis, the patient will present with signs and symptoms more consistent with impingement.
Should the biopsy be done before the steroids are started in order to ensure that the diagnosis can be made? The therapeutic effect of the steroids is necessary immediately atenolol 100 mg line pulse pressure of 80, because the second eye can become involved in as little as 24 hours generic 50mg atenolol with amex arteria obturatoria. Because skip areas also occur order atenolol 50mg without prescription blood pressure diastolic high, make sure to get a significant length of artery for biopsy buy atenolol 100 mg online hypertension nih. In a patient with less classic symptoms, a negative biopsy warrants discontinuing steroids. On examination, you find weakness of nasal eye movement in her right eye and horizontal jerk nystagmus of the left eye with attempted temporal movement. She also may have a skew deviation in which either eye can have a hypertropia that does not map to a specific muscle on the three-step test. The differential diagnoses that mimic weakness of inward eye movement include the following: & Myasthenia gravis: Ptosis and orbicularis muscle weakness are common; symptoms worsen with fatigue. An obese 30-year-old woman presents with severe headaches and occasional double vision. Check pupillary responses, color plates, visual fields, and extraocular motility; do a full slit-lamp and dilated examination. If the only abnormality is an increased opening pressure, the diagnosis is pseudotumor cerebri (Fig. Optic nerve sheath decompression is used for worsening visual fields, and lumboperitoneal shunts have been used for headaches. Drug use: Steroids (use or withdrawal), oral contraceptives, nalidixic acid, tetracycline, vitamin A 4. Patients also may have optic nerve hypoplasia in association with Goldenhar’s syndrome or septo-optic dysplasia of de Morsier. The vessels surrounding the disc are not obscured, the disc is not hyperemic, and the peripapillary nerve fiber layer is normal. Causes of pseudopapilledema include optic nerve drusen and congenitally anomalous discs. Patients have spasticity of conjugate gaze and optokinetic nystagmus abnormalities. In addition, the nasal retina is larger and allows a temporal crescent in the visual field in the contralateral eye. Patients with occipital lobe lesions often do not experience other neurologic abnormalities. If they do, they may have unformed hallucinations, dyschromatopsia, prosopagnosia, and alexia without agraphia. Pseudo–Foster Kennedy syndrome is optic atrophy with contralateral optic disc edema. The pseudosyndrome is usually the result of an acute ischemic optic neuropathy in one eye with contralateral atrophy caused by a past episode of the same process. An 18-year-old man presents with sudden vision loss in one eye, followed by the other eye within days. He has 20/20 vision in both eyes with decreased color plates and bilateral mild disc swelling with peripapillary telangiectatic microangiopathy. No effective treatment is known, but some mutations are more likely to have spontaneous improvement in the future; thus genetic evaluation of the mitochondria is worthwhile. Because patients have a higher incidence of cardiac conduction defects, referral to a cardiologist is indicated. Tearing, also called epiphora, can be caused by an increase in the amount of tears produced or by a problem with the tear drainage system. Corneal irritation can be mechanical, secondary to a tear film deficiency, or caused by exposure or allergies. Inadequate tear drainage can result from a blockage in the tear drainage system, as in punctal stenosis, canalicular stenosis, and nasolacrimal duct obstructions. Tears travel across the cornea and conjunctiva to the medial canthus, where they enter small openings in the eyelid called puncta, which are located approximately 6–7 mm from the medial canthus. The tears then enter the canaliculi, which are mucosa-lined ducts approximately 10 mm in length that carry the tears to the lacrimal sac. The first portion of the canaliculus is a 2-mm dilated, vertical segment called the ampulla. The canaliculus then bends acutely and runs parallel to the eyelid margin toward the medial canthus. In most patients the upper and lower canaliculi join to form the common canaliculus. Tears enter the lacrimal sac, which lies in a bony fossa of the medial orbital wall formed by the maxillary and lacrimal bones. It extends vertically for approximately 10 mm beginning a few millimeters superior to the medial canthal tendon and extending inferiorly to the nasolacrimal duct. The nasolacrimal duct travels through a 12-mm bony canal in the maxillary bone and then continues inferiorly for 3–5 mm before opening into the inferior meatus of the nose. It is a muscular ‘‘pump’’ that drives the tears through the drainage system by peristalsis. This forces the tears medially through the canaliculi and creates a negative pressure in the sac, drawing the tears into it. A valve between the canaliculi and sac, the valve of Rosenmuller, prevents the tears from reentering the canaliculi, so they are¨ forced down the nasolacrimal duct into the nose. The pretarsal orbicularis muscle surrounds the canaliculi and attaches to the wall of the lacrimal sac. Contraction and relaxation of this muscle help draw the tears into the canaliculus and the sac, and eventually force the tears down the nasolacrimal duct. When lower eyelid laxity is present, contraction of the orbicularis muscle does not force open the lacrimal sac, and the lacrimal pump mechanism cannot function adequately. Stretching of the medial and/or lateral canthal tendon causes lower eyelid laxity. In the distraction test, if the lower eyelid can be pulled more than 6 mm from the globe, it is lax. Poor orbicularis oculi tone, most obvious in patients with palsy of the seventh cranial nerve, also causes laxity of the lower eyelid. This is best demonstrated with the snap back test, in which the lower eyelid is pulled down inferiorly and allowed to ‘‘snap back’’ into place. If the eyelid returns to its correct position immediately, the muscle tone is good. If the patient must blink to place the eyelid back in its normal position, eyelid tone is poor. If there is laxity of the lateral canthal tendon, a horizontal lid shortening procedure is performed to tighten the eyelid. In this operation the inferior limb of the lateral canthal tendon is disinserted from the periosteum of the lateral orbital rim, and a new lateral canthal tendon is created from the lateral portion of the tarsus.
Cells have developed several carrier mechanisms to transport one solute against its concentration gradient by using the energy stored in the favorable gradient of another solute discount atenolol 50mg with mastercard blood pressure uk. In mammals order 50mg atenolol visa heart attack 90 percent blockage, most of these mechanisms use sodium as the driver solute and use the energy of the sodium gradient to carry out the “uphill” transport of another + + important solute (Fig atenolol 50 mg low price arteria coronaria izquierda. Thus 100mg atenolol with mastercard hypertension food, they are called secondary active transport mechanisms because they depend on the supply of energy to the sodium–potassium pump. Disabling the pump with metabolic inhibitors or pharmacologic blockers causes these transport systems to stop when the sodium gradient has been dissipated. A solute is moved against its concentration + + gradient by coupling it to Na moving down a favorable gradient. Binding of extracellular Na to the carrier protein (step 1) may increase the affinity of binding sites for solute, so that solute also can bind to the carrier (step 2), even though its extracellular concentration is low. A conformational change in the + carrier protein (step 3) exposes the binding sites to the cytosol, where Na readily dissociates because of + + the low intracellular Na concentration (step 4). The release of Na decreases the affinity of the carrier for solute and forces the release of the solute inside the cell (step 5), where solute concentration is already high. The free carrier then reverts to the conformation required for step 1, and the cycle begins again. Similar to passive carrier-mediated systems, secondary active transport systems are integral membrane proteins; they have specificity for the solute they transport and show saturation kinetics and competitive inhibition. First, they cannot function in the absence of the driver ion, the ion that moves along its electrochemical gradient and supplies energy. Second, they transport the solute against its own concentration or electrochemical gradient. Functionally, the different secondary active transport systems can be classified into two groups: symport (cotransport) systems, in which the solute being transported moves in the same direction as the sodium ion, and antiport (exchange) systems, in which the sodium ion and the solute move in opposite directions. Examples of symport mechanisms are the sodium-coupled sugar transport system and the several sodium-coupled amino acid transport systems found in the small intestine and the renal tubule. The symport systems allow efficient absorption of nutrients even when the nutrients are present at low concentrations. In reality, this cycle probably involves a coordinated trapping–release cycle and/or tilt of membrane-spanning segments rather than the simplistic view presented in Figure 2. These transporters have six to eight membrane-spanning segments and contain 460 to 690 amino acids. Sodium-coupled chloride transporters in the kidney are + − targets for inhibition by specific diuretics. The polypeptide chain of 664 amino acids passes back and forth across the membrane 14 times. Each membrane-spanning segment consists of 21 amino acids arranged in an α-helical conformation. In the functional protein, the membrane-spanning segments are clustered together to provide a hydrophilic pathway across the plasma membrane. The N-terminal portion of the protein, including + helices 1 to 9, is required to couple Na binding to glucose transport. The five helices (10–14) at the C terminus form the transport pathway for glucose. The first uses the sodium gradient to remove protons from the cell, controlling the intracellular pH and counterbalancing the production of protons in metabolic + reactions. The second antiporter removes calcium from the cell and, together with the different calcium pumps, helps maintain a low cytosolic calcium concentration. It is an electrogenic + 2+ system because there is a net movement of charge with three Na entering the cell and one Ca ion leaving in each cycle (Clinical Focus 2. The structures of the symport and antiport protein transporters that have been characterized (see Fig. This supports the concept that, regardless of the mechanism, the membrane-spanning regions of a transport protein form a hydrophilic pathway for rapid transport of ions and solutes across the hydrophobic interior of the membrane lipid bilayer. Although less common, malabsorption may be a direct result of a specific defect in hexose transport. Regardless of the cause, the symptoms are common and include diarrhea, abdominal pain, and gas. Some infants develop a copious watery diarrhea when fed milk that contains glucose or galactose or the disaccharides lactose and sucrose. The latter are degraded to glucose, galactose, and fructose by enzymes in the intestine. The dehydration can begin during the first day of life and can lead to rapid death if not corrected. Fortunately, the symptoms disappear when a carbohydrate-free formula fortified with fructose is used instead of milk. At least 10% of the general population has glucose or lactose intolerance, however, and it is possible that these people may have milder forms of the disease. A specific defect in absorption of glucose and galactose can be demonstrated by tolerance tests in which oral administration of these monosaccharides produces little or no increase in plasma glucose or + galactose. As these solutes accumulate in the lumen, the osmolality of the fluids increases and retards absorption of water, leading to diarrhea and severe water loss from the body. At the same time, advances in molecular biology have allowed a better understanding of the genetic defect at the cellular level and how this leads to the clinical symptoms. In a polarized cell, the entry and exit of solutes such as glucose, + amino acids, and Na occur at opposite sides of the cell. Active entry of glucose and amino acids is restricted to the apical membrane, and exit requires equilibrating carriers located only in the basolateral membrane. The result is a net movement of solutes from the luminal side of the cell to the basolateral side, ensuring efficient absorption of glucose, amino acids, + and Na from the intestinal lumen. Transcellular transport Epithelial cells occur in layers or sheets that allow the directional movement of solutes not only across the plasma membrane but also from one side of the cell layer to the other. Such regulated movement is achieved because the plasma membranes of epithelial cells have two distinct regions with different morphologies and different transport systems. These regions are the apical membrane, facing the lumen, and the basolateral membrane, facing the blood supply (Fig. The specialized or polarized organization of the cells is maintained by the presence of tight junctions at the areas of contact between adjacent cells. Tight junctions prevent proteins on the apical membrane from migrating to the basolateral membrane and those on the basolateral membrane from migrating to the apical membrane. Thus, the entry and exit steps for solutes can be localized to opposite sides of the cell. The polarized organization of the epithelial cells and the integrated functions of the plasma membrane transporters form the basis by which cells accomplish transcellular movement of both glucose and sodium ions.
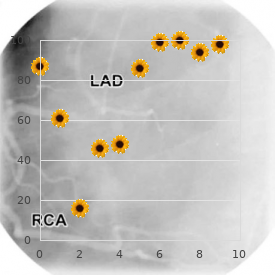
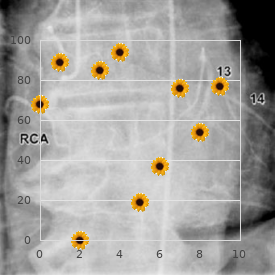
A renal biopsy and tissue examination by light and electron microscopy and immunostaining are often helpful in determining the nature and severity of the disease and in predicting its most likely course trusted 100mg atenolol arrhythmia zoloft. Poststreptococcal glomerulonephritis is an example of a nephritic condition that may follow a sore throat caused by certain strains of streptococci buy atenolol 50mg without prescription blood pressure medication not working. Immune complexes of antibody and bacterial antigen are deposited in the glomeruli generic 50 mg atenolol mastercard heart attack in men, complement is activated buy atenolol 50mg line blood pressure medication green capsule, and polymorphonuclear leukocytes and macrophages infiltrate the glomeruli. Nephrotic syndrome is a clinical state that can develop as a consequence of many different 2 diseases causing glomerular injury. Abnormal glomerular leakiness to plasma proteins leads to increased proximal tubular reabsorption and catabolism of filtered proteins and increased protein excretion in the urine. The resulting loss of protein (mainly serum albumin) leads to a fall in plasma protein concentration (and colloid osmotic + pressure). Also, a generalized increase in capillary permeability to proteins (not just in the glomeruli) may lead to a decrease in the effective colloid osmotic pressure of the plasma proteins and may contribute to the edema. The hyperlipidemia (elevated serum cholesterol and elevated triglycerides in severe cases) is probably a result of increased hepatic synthesis of lipoproteins and decreased lipoprotein catabolism. Most often, nephrotic syndrome in young children cannot be ascribed to a specific cause; this is called idiopathic nephrotic syndrome. Nephrotic syndrome in children or adults can be caused by infectious diseases, neoplasia, certain drugs, various autoimmune disorders (such as lupus), allergic reactions, metabolic disease (such as diabetes mellitus), or congenital disorders. The distinctions between nephritic and nephrotic diseases are sometimes blurred, and both may result in chronic glomerulonephritis. This disease is characterized by proteinuria and/or hematuria (blood in the urine), hypertension, and renal insufficiency that progresses over years. Renal biopsy shows glomerular scarring and increased numbers of cells in the glomeruli and scarring and inflammation in the interstitial space. The disease is accompanied by a progressive loss of functioning nephrons and proceeds relentlessly even though the initiating insult may no longer be present. The exact reasons for disease progression are not known, but an important factor may be that surviving nephrons hypertrophy when nephrons are lost. This leads to an increase in blood flow and pressure in the remaining nephrons, a situation that further injures the glomeruli. Also, increased filtration of proteins causes increased tubular reabsorption of proteins, and the latter results in production of vasoactive and inflammatory substances that cause ischemia, interstitial inflammation, and renal scarring. Dietary manipulations (such as a reduced protein intake) or antihypertensive drugs (such as angiotensin- converting enzyme inhibitors) may slow the progression of chronic glomerulonephritis. Glomerulonephritis in its various forms is the major cause of renal failure in people. No active transport mechanisms are involved in moving the fluid from the plasma across the glomerular filtration barrier into the lumen of the Bowman capsule. Since the glomerulus is a tuft of capillaries, the same hemodynamic forces apply here that causes ultrafiltration across other capillaries (see Chapter 15). Glomerular hemodynamics are characterized by high capillary pressure and low vascular resistance. Note that average capillary hydrostatic pressure in the glomerulus is much higher than in a skeletal muscle capillary (55 vs. Also, capillary hydrostatic pressure declines little (perhaps 1 to 2 mm Hg) along the length of the glomerular capillary, because the glomerulus contains many (30 to 50) capillary loops in parallel, thereby making the resistance to blood flow in the glomerulus low. In the skeletal muscle capillary, there is a much higher resistance to blood flow, resulting in an appreciable fall in capillary hydrostatic pressure with distance. In the normal human glomerulus, filtration probably occurs along the entire capillary. Assuming that K is uniform along the length of the capillaryf, filtration rate would be highest at the afferent arteriolar end and lowest at the efferent arteriolar end of the glomerulus. Glomerular capillary pressure is the major force that determines glomerular filtration. This pressure ultimately depends on the blood pressure on the arterial side of the circulation. Normally, about 20% of the plasma flowing through the kidneys is filtered in the glomeruli. Changes in filtration fraction will result from constriction or dilation of afferent or efferent arterioles. For example, afferent arteriolar dilation or efferent arteriolar constriction leads to an increase in filtration fraction. Capillary osmotic pressure and hydrostatic pressure in the Bowman capsule oppose glomerular filtration. It also provides the driving force for fluid movement down the length of the tubule. If tubular reabsorption of water is inhibited, pressure in the tubular system is increased because an increased pressure head is needed to force a large volume flow through the loops of Henle and collecting ducts. Glomerular ultrafiltration coefficient depends on the properties of the glomerular filtration barrier. The glomerular ultrafiltration coefficient (K )f is the glomerular equivalent of the capillary filtration coefficient encountered in Chapter 15. Accordingly, K depends on both membrane permeability andf surface area of the glomerular filtration barrier. Compared to typical systemic capillaries, the normal Kf for the glomerulus is very high. Compared with most other capillaries, the glomerular capillaries behave as though they have more pores per unit surface area; consequently, they have an unusually high hydraulic conductivity. Capillary hydrostatic pressure is higher in the glomeruli than in any other capillaries. In conclusion, glomerular filtration is high because the glomerular capillary blood is exposed to a large, porous surface and there is a high transmural pressure gradient favoring filtration. When the filtration membrane is not functioning properly, it ceases to be an effective barrier. What then occurs is proteinuria, an abnormal accumulation of protein in the urine. A very small amount of protein gets filtered normally (~5 to 20 mg/d), but this is almost completely reabsorbed in the proximal tubule by endocytosis. If protein is detected in the urine, it usually means that there is a breakdown in the filtration barrier. Proteinuria not only is a sign of kidney disease but also results in tubular and interstitial damage and contributes to the progression of chronic renal disease. This is due to the fact that high levels of proteins in the filtrate have a pathogenic effect on the renal tubules.